Description
Disclaimer: Copyright infringement not intended
Context
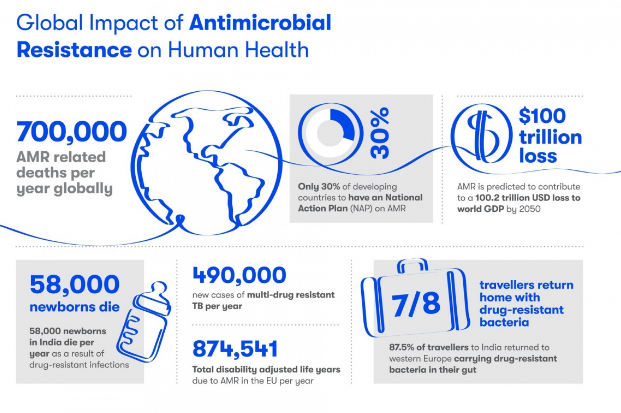
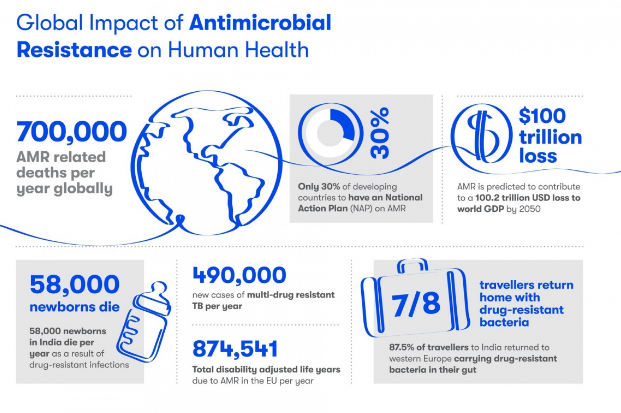
- 27 million people died in 2019 as a direct result of AMR, which is now a leading cause of death worldwide, higher than HIV/AIDS or malaria - Global Research on Antimicrobial Resistance (GRAM) report.
- The Global Research on Antimicrobial Resistance (GRAM) report used statistical modelling to estimate deaths linked to 23 pathogens and 88 pathogen-drug combinations.
|
GRAM
GRAM is the flagship project of the University of Oxford Big Data Institute–IHME Strategic Partnership. GRAM was launched with support from the United Kingdom Department of Health’s Fleming Fund, the Wellcome Trust, and the Bill & Melinda Gates Foundation.
The purpose of the Global Research on AntiMicrobial resistance (GRAM) Project is to generate accurate and timely estimates of the magnitude and trends in antimicrobial resistance (AMR) burden across the world.
Importance: This data can be used to inform treatment guidelines and agendas for decision-making and research, detect emerging problems and monitor trends to inform global strategies, as well as facilitate the assessment of interventions over time.
|
What are antimicrobials?
- Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitics – are medicines used to prevent and treat infections in humans, animals and plants.
What is antimicrobial resistance?
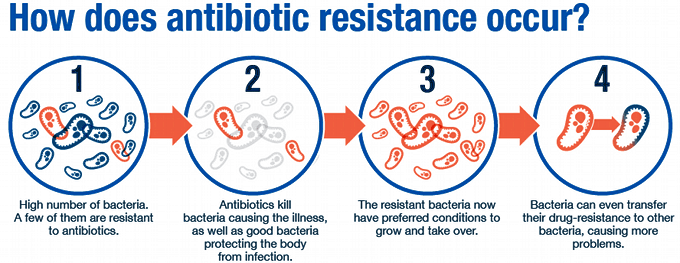
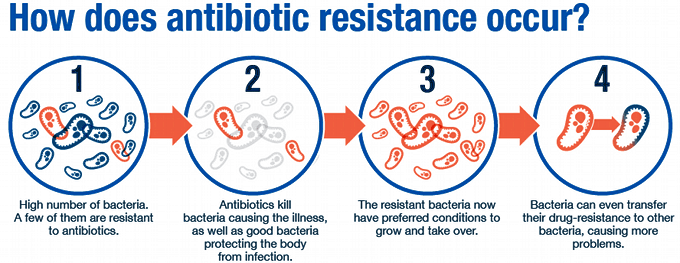
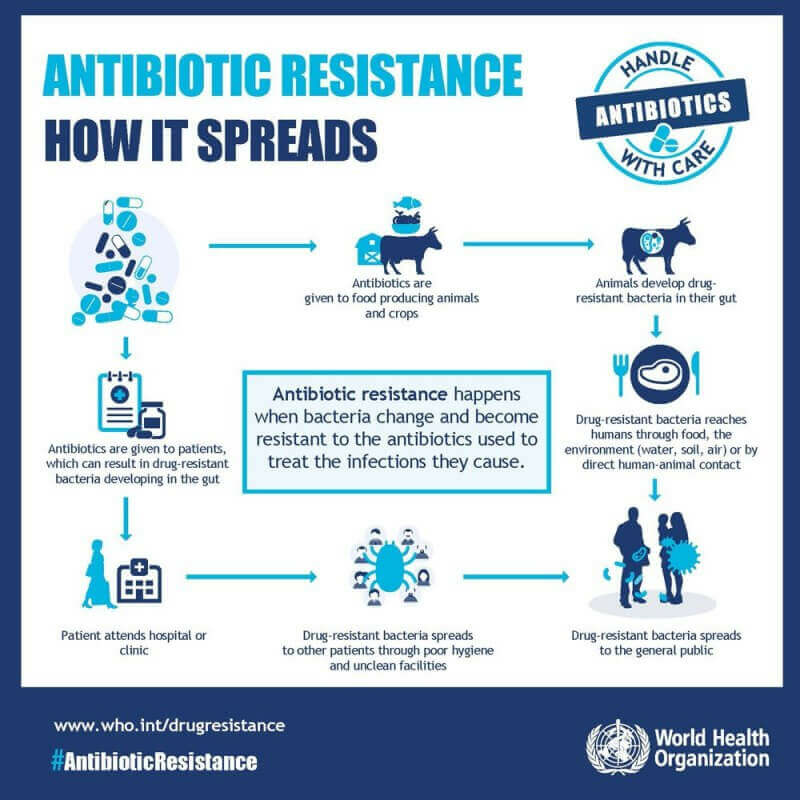
- AMR happens when microorganisms (such as bacteria, fungi, viruses, and parasites) change and are still able to grow, even when they are exposed to antimicrobial medicines that are meant to kill or limit their growth (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics).
- As a result, the medicines become ineffective and infections persist in the body, increasing the risk of spread to others.
Factors leading to AMR
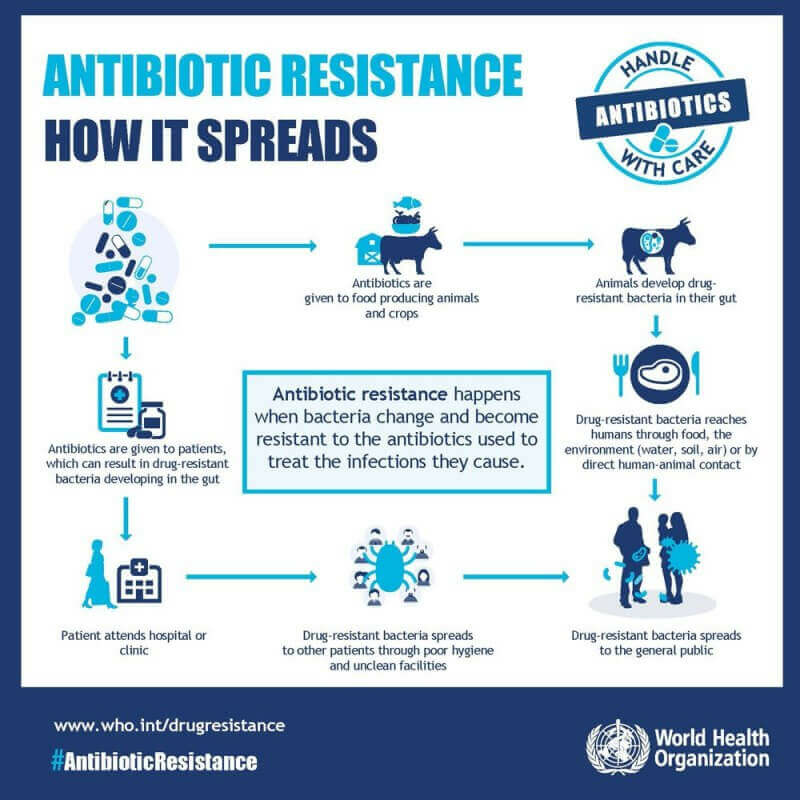
- The main drivers of antimicrobial resistance include the
- Misuse and overuse of antimicrobials;
- Lack of access to clean water,
- Sanitation and hygiene (wash) for both humans and animals;
- Poor infection and disease prevention and control in health-care facilities and farms;
- Poor access to quality, Affordable medicines, Vaccines and diagnostics;
- Lack of awareness and knowledge; and Lack of enforcement of legislation.
- Lack of access to timely and appropriate treatments for infections,
- Self-medication, prescription sharing, over-the counter sale of antimicrobials,
- Non-compliance with the prescribed treatment.
- genetic mutation of bacteria.
- By one species acquiring resistance from another.

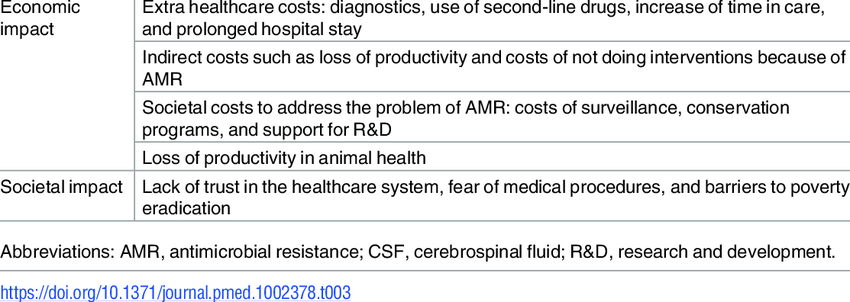
Impact of AMR
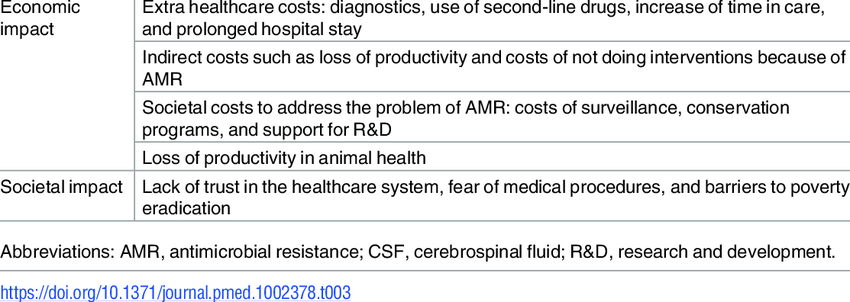
Statistics
- India is one of the largest consumers of antibiotics in the world.
- Antibiotic use in India has risen sharply, with about a 30% increase in their per capita use during the past decade, according to the State of the World’s Antibiotics 2021 report.
- 5 lakh people die annually due to AMR worldwide.
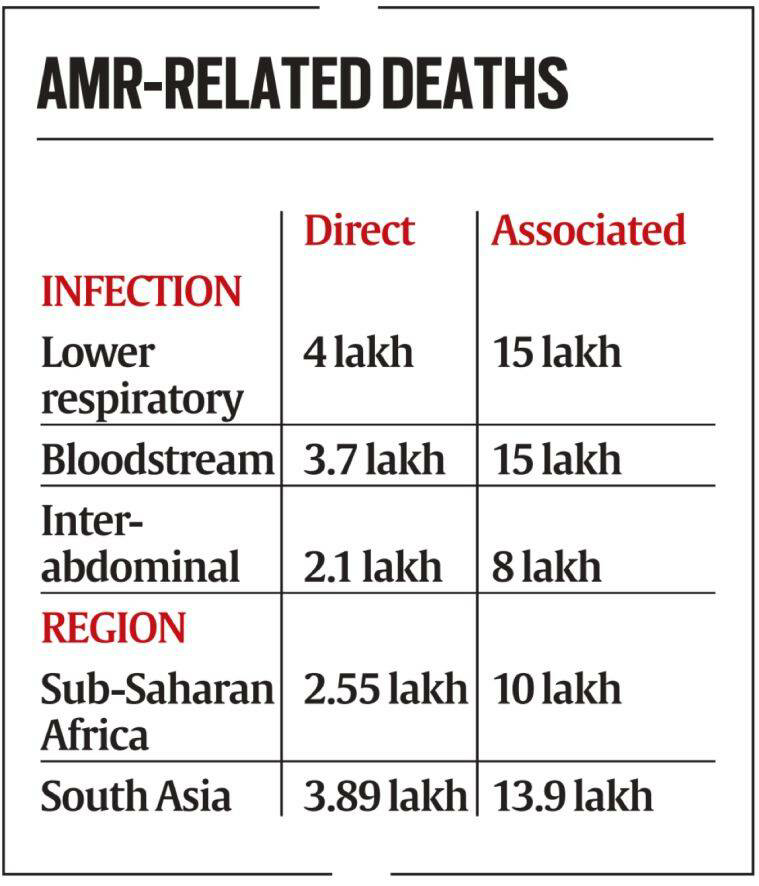
Findings of the GRAM report
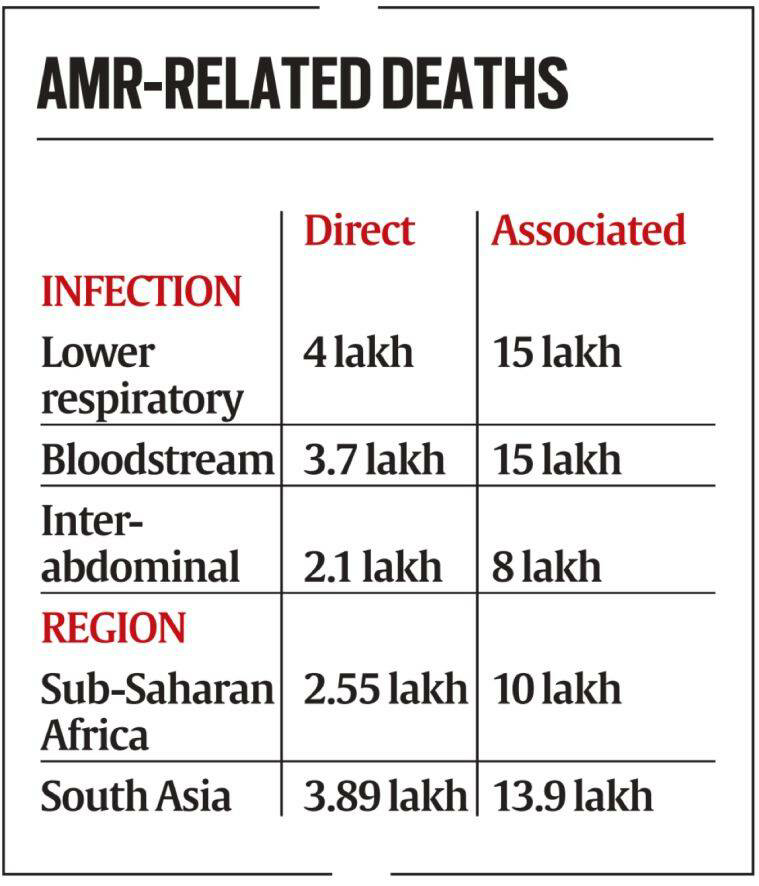
- Of the 23 pathogens studied, drug resistance in six (E coli, S aureus, K pneumoniae, S pneumoniae, A baumannii, and P aeruginosa) led directly to 9.29 lakh deaths and was associated with 3.57 million.
- One pathogen-drug combination – methicillin-resistant S aureus, or MRSA – directly caused more than 1 lakh deaths.
- Resistance to two classes of antibiotics often considered the first line of defence against severe infections – fluoroquinolones and beta-lactam antibiotics – accounted for more than 70% of deaths caused by AMR.
- 10-fold: Variation between countries in total antibiotic consumption rates, ranging from as low as 5 DDD to 45.9 DDD per 1000 population per day.
- 46% up: Between 2000 and 2018, global antibiotic consumption rates increased from 9.8 to 14.3 DDD per 1000 population per day).
- 76%: Increase observed between 2000 and 2018 in low- and middle-income countries (from 7.4 to 13.1 DDD per 1000 per day). In high-income countries, consumption rates remained stable.
- 116%: Increase in antibiotic consumption rates in South Asia. The second largest increase was in the North Africa and Middle East region (111%).
Steps taken to curb AMR in India
Red Line Campaign
- It urges people not to use medicines marked with a red vertical line, including antibiotics, without a doctor’s prescription. These medicines are called as the ‘Medicines with the Red Line’.
National Action Plan on Antimicrobial Resistance
- India has a National Action Plan on Antimicrobial Resistance in place
Delhi Declaration on Antimicrobial Resistance
- Delhi Declaration on Antimicrobial Resistance, was endorsed at the Inter-Ministerial Consultation on Antimicrobial Resistance in 2017.
AMR Surveillance Network
- ICMR has established AMR surveillance and research network (AMRSN) in 2013, to generate evidence and capture trends and patterns of drug resistant infections in the country.
- This network comprises of 30 tertiary care hospitals, both private and government.
AMR Research & International Collaboration
- ICMR has taken initiatives to develop new drugs /medicines through international collaborations in order to strengthen medical research in AMR.
- ICMR along with Research Council of Norway (RCN) initiated a joint call for research in antimicrobial resistance in 2017.
- ICMR along with Federal Ministry of Education and Research (BMBF), Germany has a joint Indo-German collaboration for research on AMR.
Initiatives to control overuse or misuse of antibiotics
- ICMR has initiated antibiotic stewardship program (AMSP) on a pilot project basis in 20 tertiary care hospitals across India to control misuse and overuse of antibiotics in hospital wards and ICUs.
- On the recommendations of ICMR, DCGI has banned 40 fixed dose combinations (FDCs) which were found inappropriate.
- ICMR worked in collaboration with Indian Council of Agriculture Research, Department of Animal Husbandry, Dairy and Fisheries and the DCGI to ban use of Colistin as growth promoter in animal feed in poultry.
Guidelines issued
- National Guidelines for Infection Prevention and Control in Healthcare Facilitie shave been released by MoHFW in Jan 2020.
- ICMR has developed evidence based treatment guidelines for treatment of ten syndromes of infections. It aims to rationalize the usage of antibiotics on Essential Medicines Formulary (EMF) and to establish consistency in the treatment of various infectious conditions.
- Further, ICMR has also issued the Treatment Guidelines for Antimicrobial Use in Common Syndromes” in 2019.
Way Ahead
- Lowering of antibiotic consumption is not sufficient because the spread of resistant strains and resistance genes are the dominant contributing factor.
- Providing sanitation, clean water and good governance, increasing public health expenditure and better regulating the private health sector are all necessary to reduce antimicrobial resistance.
https://indianexpress.com/article/explained/explained-global-toll-bacterial-resistance-to-drugs-7732479/