Description
Disclaimer: Copyright infringement not intended.
Context: A study on COVID-19 by the Indian Council of Medical Research was published recently
Findings of the study
- The study includes patients who were hospitalized since September 2020, meaning the infections are likely to have been caused by the original, delta, or omicron coronavirus variants.
- The study found that 1% of the participants experienced post-COVID-19 conditions such as lethargy and breathlessness, and cognitive abnormalities like brain fog and difficulty in concentrating.
- The people were nearly three times more likely to die if they experienced these post-Covid-19 conditions.
- Nearly 6.5% of people hospitalized with Covid-19 died in the following year.
- The study also showed that even a single dose of the vaccine before the infection reduced the number of deaths in the one-year period by 60%.

Who was at higher risk of mortality?
- The factors that increased the risk of death later in the year following a COVID-19 infection were comorbidity, age, and gender.
- People with one comorbid condition were more than 9 times more likely to die during the year following the infection.
- Men were 1.3 times more likely to die and those above the age of 60 years were 2.6 times more likely to die.
- Children between the ages of 0 and 18 years were at a 5.6 times higher risk of death between the first follow-up at four weeks and the follow-up at the one-year mark.
- Comorbidities among admitted children are more severe, such as malignancies, kidney disorders, hematological disorders and others.
- People with any comorbidities, especially conditions such as liver cirrhosis and chronic kidney disease, must take all precautions because they are likely to get severe disease and complications.
The post-Covid-19 conditions
- Post COVID-19 Condition, commonly known as long COVID, can affect anyone exposed to SARS-CoV-2, regardless of age or severity of original symptoms.
- It is defined as the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least 2 months with no other explanation.
- The study did not use the exact definition of “post-Covid-19 conditions”, given by the World Health Organization or Centers for Disease Control and Prevention (CDC) as they came out after patient enrolment had already begun.
- The ICMR study defines “Covid-19 conditions” as persistent or new onset of fatigue, breathlessness, or cognitive abnormalities.
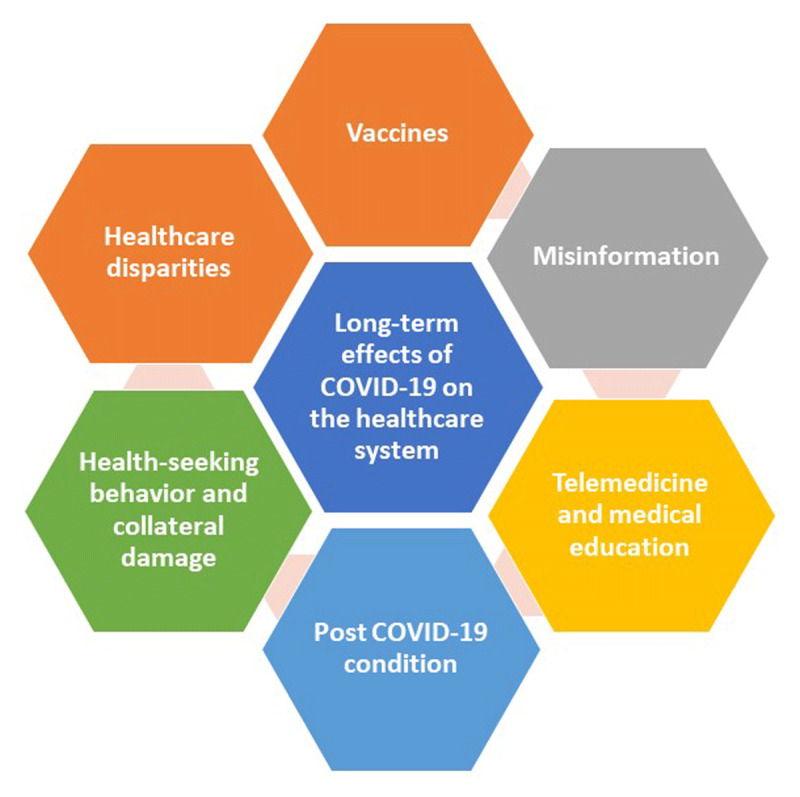
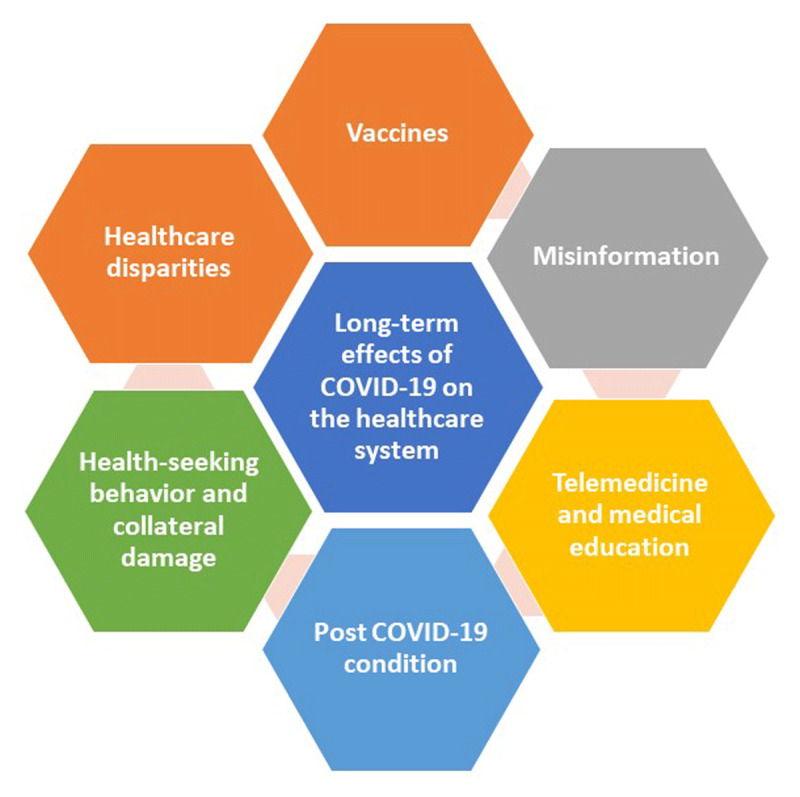
Fig: The long-term effects of the coronavirus disease 19 (COVID-19) pandemic on the healthcare system.
Way ahead to prepare for post-Covid scenario
Vaccines
- Since the beginning of the pandemic, there have been accelerated efforts to sequence the genetic material of the virus and build effective vaccines that decrease the risk of infection, hospitalization, and mortality.
- More recently, booster doses have been administered. The rate of recurrence after the second or booster doses also is unclear. There is a need to prepare infrastructure for the development of vaccines in future.
Combating Misinformation
- Since the beginning of the pandemic, misinformation has spread throughout the Internet and on social media platforms.
- Tackling this will require concerted efforts by the government and private sector, particularly social media companies, to implement evidence-based communication strategies. Individuals should also assume responsibility for seeking out accurate, evidence-based information for their consumption.
Telemedicine
- In 2020, telemedicine was the main means by which ambulatory care was provided, accounting for 10% to 20% of visits when virus transmissibility was low and as high as 80% of visits during the surges. Given this data telemedicine should be leveraged
Post Covid-19 Condition
- There is a growing body of evidence that some patients have prolonged recovery and/or residual symptoms after acute infection with COVID-19.
- Recent data also suggests that post-COVID-19 conditions might not be limited to somatic symptoms, with studies showing a 7-fold increased risk of developing depression and mental health issues. More research in this area is needed.
Disparities in Healthcare
- The pandemic exposed significant disparities in healthcare delivery, particularly among minorities. Understanding the disparities and identifying measures to bridge the gap will be an important area of research for policy.
Changes to Medical Education
- There is a need for significant changes to both graduate and continued medical education.
Conclusion
- The COVID-19 pandemic has dramatically changed clinical practice, medical education, and research. Beyond the immediate increase in morbidity and mortality, the healthcare system is having to deal with a growing cohort of patients with lingering symptoms. Misinformation, vaccine hesitancy, and vaccine inequity will be continuing challenges to attaining herd immunity.
- Clinicians, educators, and healthcare administrators will also have to determine how best to leverage the transition to virtual platforms. Lastly, healthcare leaders and policymakers will have to help the country and world chart a course through the end of the pandemic.
|
PRACTICE QUESTION
Q. The Covid-19 pandemic might have been prevented but the post-Covid scenario grapples with multiple challenges in terms of healthcare infrastructure, misinformation, vaccine hesitancy, vaccine inequity and post-covid conditions. Critically analyse. ( 250 words)
|
https://indianexpress.com/article/explained/explained-health/icmr-study-on-long-covid-what-are-its-key-findings-8908222/