Description

Disclaimer: Copyright infringement not intended.
Context: Union Health & Family Welfare Minister Mansukh Mandaviya declared that India is committed to eradicating Lymphatic Filariasis by 2027, surpassing the global target by three years.
Lymphatic Filariasis
- Filariasis is a disease caused by a chronic mosquito-borne parasitic infection. Chronic infection can lead to swelling of the extremities, hydroceles, and testicular masses.
- It is the second-largest cause of permanent deformity and disability behind leprosy worldwide.
- Lymphatic filariasis is a neglected tropical disease that causes significant morbidity in the developing world.
- The Global Programme to Eliminate Lymphatic Filariasis is providing mass drug administrations (MDA) to populations in endemic areas in a push to eradicate this disease.
Etiology
- Causes- Three species of nematode parasites: Wuchereria bancrofti, Brugia malayi, and Brugia timori
- Vectors- Aedes, Anopheles, Culex, Mansonia, and Ochlerotatus.
Epidemiology
- It affects 120 million people in 72 countries worldwide, mostly in the tropics and subtropical climates of Asia, Africa, the Western Pacific, South America, and the Caribbean.
- Four countries in America are endemic: Haiti, Dominican Republic, Guyana, and Brazil.
- One-third of children in endemic regions are asymptomatically infected with W. bancrofti.
- Half of the patients infected are in their 30s or 40s, and there is a 10:1 predilection for men to women.

Trend and present endemicity of filariasis in India
- The estimates in 2001 indicate that about 473 million people are exposed to the risk of bancroftian infection and of these about 125 million live in urban areas and about 348 million in rural areas.
- About 31 million people are estimated to be harbouring microfilaria (mf) and over 23 million suffer from filaria disease manifestations.
- The state of Bihar has the highest endemicity (over 17%) followed by Kerala (15.7%) and Uttar Pradesh (14.6%).
- B malayi nocturnal periodic infection is prevalent in the states of Kerala, Tamil Nadu, Andhra Pradesh, Orissa, Madhya Pradesh, Assam and West Bengal. The single largest tract of this infection lies along the west coast of Kerala.
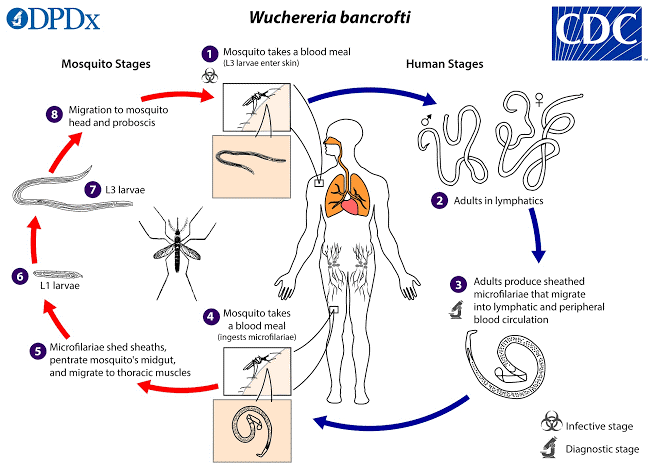
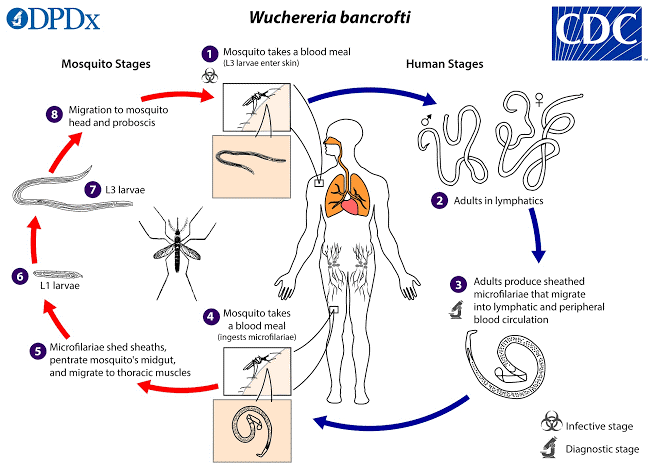
Pathophysiology
- Humans are the primary reservoir for this parasitic disease, and mosquitoes are the vector.
- The mosquito deposits larvae into the bloodstream.
- They take up residence in the lymph nodes and grow into adult worms.
- The larvae have a predilection to deposit in femoral lymph nodes.
- They undergo sexual reproduction, and females give birth to countless microfilariae, which are dumped into circulation in a diurnal pattern.
- The proliferation of adult worms disrupts the lymphatic drainage and increases the susceptibility to repeated infections - most notably streptococcal and fungal infections.
Main challenge
- The major challenge with the currently available drugs is that the interruption of transmission requires very high treatment coverage (probably > 85% of the total population) to achieve elimination.
- Current approaches to drug delivery do not achieve this (only 40-60% get treated if mass treatment is executed by regular health services).
- There is an urgent need for more effective drug delivery strategies for lymphatic filariasis elimination that are adapted to regional differences and variations in health sector development.
Filariasis Control in India
- After a pilot project in Orissa from 1949 to 1954, the National Filaria Control Programme (NFCP) was launched in the country in 1955, to delimit the problem, to undertake control measures in endemic areas and to train personnel to man the programme.
- The main control measures were mass DEC administration, antilarval measures in urban areas and indoor residual spray in rural areas.
- The revised program was launched in 1996-97 in 13 districts in seven endemic states namely Andhra Pradesh, Bihar, Kerala, Orissa, Uttar Pradesh, Tamil Nadu and West Bengal, where MDA was undertaken.
- India is committed to eliminating Lymphatic Filariasis by 2027, three years ahead of the global target through mission mode, multi-partner, multi-sector, targeted drive for which we have drawn up the roadmap”.
Way ahead
- Efforts shouldn't merely be focused on medication but also on curbing disease transmission via mosquitoes.
- Enhanced synergy between state and central governments is the need of the hour.
- Community engagement plays a pivotal role. Ex. Health initiatives like the Ni-kshay Mitra spotlighted the impact of grassroots involvement in health missions.
- The "Whole of Government" and "Whole of Society" approach is pivotal to successfully eliminating the disease.
- Awareness campaigns at local levels, such as villages and panchayats are pivotal.
- Given the significance of diligent medicine consumption, it is recommended that the medication be done under the watch of healthcare professionals to ensure efficacy.
- Second phase of the Annual Nationwide Mass Drug Administration (MDA) initiative.
- National Guidelines for Clinical Management of Dengue and Chikungunya Fevers for 2023.
Conclusion
- Better diagnostics and procedures need to be developed for monitoring and surveillance. Research is required on the progression and reversibility of disease manifestations, especially in children and after (mass) treatment. Another priority is the development of new drugs or drug combinations for curative treatment or sustained suppression of the (larval) microfilariae forms of the parasite.
|
PRACTICE QUESTION
Q. India is committed to eliminating Lymphatic Filariasis by 2027, three years ahead of the global target. However, the road to achieve the target is tough and multiplicity of efforts are required. Critically analyze.(250 Words)
|
.jpg)
https://www.livemint.com/news/india/india-committed-to-eliminate-lymphatic-filariasis-by-2027-mandaviya-11691665502226.html