Description

Copyright infringement not intended
Picture Courtesy: https://www.telegraphindia.com/opinion/gulp-it-down-editorial-on-centres-minimal-fund-hike-in-midday-meal-schemes/cid/1891517
Context: The Lancet study highlights a dual health challenge in India with a significant increase in obesity among both adults and children over the past 32 years, coexisting with a persistent prevalence of undernutrition, creating a "double burden" on the country's health system.
Details
- The Lancet study spanning 32 years reveals a sustained and concerning upward trend in obesity levels among both adults and children in India, posing a significant public health challenge as obesity is closely linked to an increased risk of various non-communicable diseases, including diabetes, hypertension, heart disease, and strokes.
- The study underscores the role of increased consumption of processed foods, rich in fats, salt, and sugar, in driving the obesity epidemic in India, emphasizing the crucial link between dietary choices and the availability of food options with public health outcomes.
- The parameters for being obese and underweight are defined based on Body Mass Index (BMI), a commonly used indicator of body fatness. The World Health Organization (WHO) provides guidelines for BMI classification, and these standards are widely used by health organizations globally.

Obesity
- Obesity is characterized by an abnormal or excessive accumulation of fat that poses health risks.
- Adults (20 years and older): Considered obese if their Body Mass Index (BMI) is 30 kg/m² or more.
- School-aged children and adolescents (5 to 19 years): Considered obese if their BMI is two standard deviations above the mean for their age group.
- BMI is calculated using the formula: BMI = Weight (kg) / (Height (m))^2.
- For adults, a BMI of 30 kg/m² or higher is the threshold for obesity.
- For children and adolescents, the BMI is compared to age-specific reference charts, and a value two standard deviations or more above the mean indicates obesity.
|
Obesity Trends
●Women: There has been a substantial increase in obesity among women, with the prevalence rising from 1.2% in 1990 to 9.8% in 2022. The absolute number of women living with obesity in 2022 reached 44 million.
●Men: Obesity in men also increased by 4.9 percentage points during the same period. In 2022, there were 26 million men living with obesity.
●Childhood Obesity: The study reveals a significant increase in childhood obesity over the 32-year period. In 2022, 3.1% of girls and 3.9% of boys were classified as obese. The absolute numbers indicate a substantial rise, with millions of boys and girls being obese in 2022.
|
Underweight
- Underweight is one of the four broad sub-forms of undernutrition, indicating insufficient body weight for a given height.
- Adults (20 years and older): Considered underweight if their BMI is less than 18 kg/m².
- School-aged children and adolescents (5 to 19 years): Considered underweight if their BMI is two standard deviations below the mean for their age group.
- BMI is calculated using the same formula: BMI = Weight (kg) / (Height (m))^2.
- For adults, a BMI below 18 kg/m² indicates underweight.
- For children and adolescents, the BMI is compared to age-specific reference charts, and a value two standard deviations or more below the mean indicates underweight.
|
Underweight and Thinness Trends
●Overall Prevalence: Despite the rise in obesity, the prevalence of underweight and thinness remains high across genders and age groups.
●Women and Men: 13.7% of women and 12.5% of men were classified as underweight.
●Childhood Thinness: Thinness in children, particularly girls, is a significant concern.
●Indian girls have the highest prevalence of thinness globally, with a rate of 20.3%.
●Indian boys have the second-highest prevalence of thinness globally, with a rate of 21.7%.
|
Factors contributing to the higher prevalence of obesity in women compared to men in India
- Lack of Physical Activity: Women may face challenges in accessing or dedicating time to physical activities like walks or going to gyms. Limited physical activity is a significant contributor to weight gain and obesity.
- Prioritizing Family Nutrition: Women, being primary caregivers in many households, often prioritize the nutritional needs of their family over their own. This prioritization might lead to dietary choices that are less conducive to personal weight management.
- Sleep Patterns: Women may experience disrupted sleep patterns, waking up early and going to bed late. Inadequate or irregular sleep can negatively impact metabolism and contribute to weight gain.
- Central Obesity: The concept of central obesity, which refers to an excess accumulation of fat in the abdominal area. Central obesity is considered a more accurate predictor of future risks of diseases like diabetes and hypertension than overall obesity.
- Socio-economic Factors: Though not explicitly mentioned, socio-economic factors could play a role. Women's access to resources, including opportunities for physical activity and healthier food choices, may be influenced by their socio-economic status.
- Cultural and Societal Norms: Cultural expectations and societal norms may shape women's roles and responsibilities. These norms could impact the time available for self-care activities such as exercise and sleep.
|
●The higher prevalence of obesity in women has significant health implications, as obesity is associated with an increased risk of various health conditions, including diabetes and hypertension.
●Understanding the multifaceted factors contributing to gender-specific obesity trends is crucial for developing effective public health strategies. Interventions should be tailored to address the unique challenges faced by women in maintaining a healthy lifestyle.
|
Patterns of obesity and undernutrition in India
- Shift in Obesity Trends: The Lancet study highlights a shift in obesity trends in India, noting that while traditionally associated with affluence, economic factors have made it more prevalent among the economically disadvantaged. This shift is attributed to the affordability and accessibility of unhealthy processed foods, like samosas and pakoras, compared to fresh fruits and vegetables, emphasizing the significant impact of economic dynamics on obesity prevalence.
- Rural-Urban Divide: Urban areas experience higher prevalence rates of obesity compared to rural areas. Urban settings may offer easier access to a variety of food options, including processed and fast foods. Sedentary lifestyles and desk jobs prevalent in urban areas may contribute to higher obesity rates.
- Undernutrition in Poor and Remote Regions: Despite the rise in obesity, undernutrition persists in extremely remote and rural parts of economically poorer states. States like Bihar, Jharkhand, or Odisha face high rates of undernutrition, where some individuals may struggle to afford and access an adequate number of meals.
- Economic Factors Impacting Food Choices: Economic constraints heavily influence food choices. Unhealthy, processed foods are often more cost-effective and may be perceived as tastier than healthier alternatives.
- Global Comparison: The comparison with the West highlights a global trend where unhealthy food options tend to be more affordable than fresh and nutritious alternatives.
- Public Health Implications: The coexistence of obesity and undernutrition creates a dual burden of malnutrition in India. Some segments of the population face challenges of overconsumption, while others struggle with limited access to sufficient and nutritious meals.
|
Effective public health policies must address the socio-economic determinants of health. Strategies may include promoting healthier and more affordable food options, improving access to nutritious meals in rural areas, and raising awareness about balanced diets.
|
Consequences of the Double Burden
Individual Health Implications
- Increased Risk of Non-Communicable Diseases (NCDs): Individuals experiencing both undernutrition and obesity are at a heightened risk of developing NCDs, such as diabetes, hypertension, and cardiovascular diseases. The combination of malnutrition can lead to a range of metabolic and cardiovascular complications.
- Compromised Immune Function: Undernutrition weakens the immune system, making individuals more susceptible to infections and illnesses. Obesity, on the other hand, can lead to chronic inflammation, further compromising immune function.
- Stunted Development in Children: The coexistence of undernutrition and obesity in children can result in stunted physical and cognitive development. Children may face both short-term and long-term health challenges.
- Psychosocial Impact: Individuals experiencing the double burden may face psychosocial challenges, including body image issues and mental health concerns. Societal stigmas associated with weight can contribute to mental health issues.
Economic Burden
- Increased Healthcare Costs: The presence of both undernutrition and obesity contributes to a higher burden on the healthcare system. Treatment and management of NCDs associated with obesity require significant healthcare resources.
- Productivity Loss: Health issues arising from the double burden can lead to reduced productivity among the workforce. Absenteeism and decreased work efficiency contribute to economic losses for both individuals and the nation.
- Intergenerational Impact: Stunted development in children can have intergenerational effects, perpetuating a cycle of health challenges and economic disadvantages.
Public Health Challenges
- Strained Healthcare Systems: The dual burden poses challenges for healthcare systems, as they must address the diverse and sometimes conflicting nutritional needs of the population. Resource allocation and planning become more complex.
- Complicated Intervention Strategies: Designing and implementing effective public health interventions becomes more challenging when addressing both undernutrition and obesity simultaneously. Interventions must be tailored to the specific needs of different population segments.

Social Inequality and Disparities
- Socio-economic Divide: The double burden often reflects and exacerbates existing socio-economic disparities. Vulnerable populations may face challenges accessing healthcare, nutritious food, and educational resources.
- Impact on Women: Women, who may be disproportionately affected by both undernutrition and obesity, face unique challenges related to reproductive health, maternal health, and overall well-being.
Way Forward
- Nutrition Education and Awareness: Raise awareness about the importance of balanced nutrition. Educate communities about the risks of both undernutrition and overnutrition. Promote healthy eating habits, portion control, and the significance of diverse diets.
- Promotion of Breastfeeding: Encourage and support breastfeeding, as it provides essential nutrients for infants and contributes to their healthy growth and development. Disseminate information on the benefits of exclusive breastfeeding during the first six months of life.
- Access to Nutrient-Dense Foods: Improve access to affordable, nutrient-dense foods, especially for vulnerable populations. Enhance agricultural practices and food production to ensure a diverse and nutritious food supply.
- Public Health Interventions: Implement policies to reduce the consumption of unhealthy foods and beverages. Implement sugar taxes, food labelling, and other regulatory measures to discourage the intake of high-calorie, low-nutrient foods.
- Healthcare Services and Monitoring: Strengthen healthcare systems to identify and address both undernutrition and overnutrition. Monitor and evaluate the nutritional status of populations regularly to identify trends and areas for intervention.
- Social Safety Nets: Establish and strengthen social safety nets to provide support for vulnerable populations, ensuring access to nutritious foods. Address socio-economic factors that contribute to malnutrition, such as poverty and inequality.
- Community Engagement: Engage communities in the design and implementation of nutrition programs. Empower individuals to make informed choices regarding their nutrition and that of their families.
- Collaboration and Partnerships: Foster collaboration among government agencies, non-governmental organizations, the private sector, and international bodies to create a coordinated response. Share best practices and lessons learned from successful interventions in different regions.
- Research and Innovation: Invest in research to better understand the causes and consequences of the double burden of malnutrition. Promote innovation in food production, distribution, and dietary practices to address emerging challenges.
- Policy Integration: Integrate nutrition considerations into broader policies related to health, agriculture, education, and social development. Ensure coherence between different policy areas to create a supportive environment for nutritional well-being.
|
Malnutrition in India
|
|
Key Points
|
Description
|
|
Prevalence
|
●According to the latest National Family Health Survey (NFHS-5, 2019-21), 20.3% of girls and 21.7% of boys under five are wasted (indicating low weight for height) - the highest rates globally. Furthermore, 35.5% of children under-five and 13.7% of women are underweight.
●The NFHS-5 data reveals that 28.6% of urban men and 31.7% of urban women are overweight or obese, compared to 18.8% and 19.0% in rural areas, respectively.
|
|
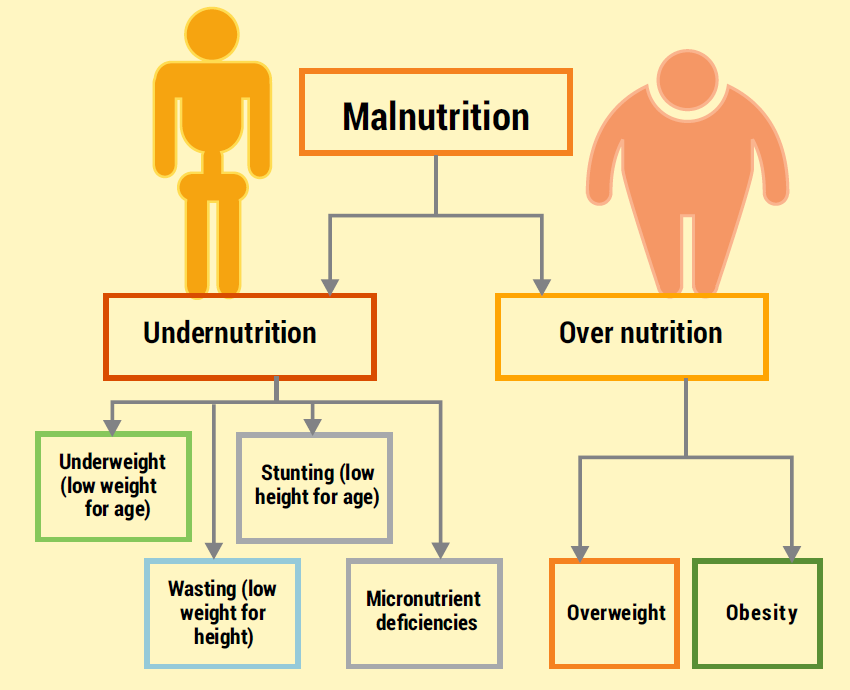
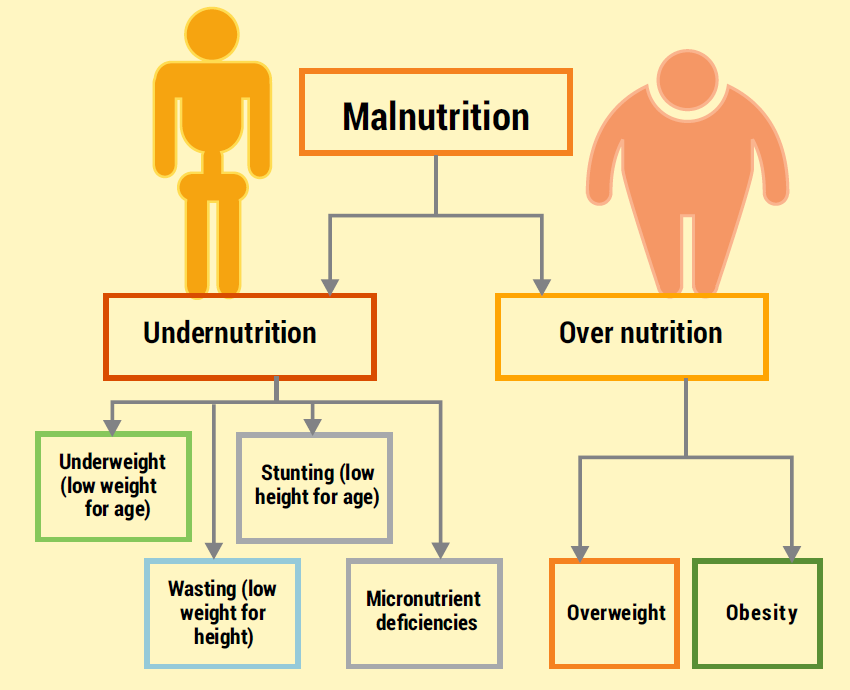
Types of Malnutrition
|
●Undernutrition: This includes stunting (low height for age), wasting (low weight for height), and underweight (low weight for age) among children, indicating chronic malnutrition.
●Micronutrient Deficiency: Common deficiencies include iron, vitamin A, and iodine, leading to various health issues.
●Overnutrition: This refers to the rising prevalence of overweight and obesity, particularly in urban areas, driven by factors such as unhealthy dietary habits and sedentary lifestyles.
|
|
Causes
|
●Poor Dietary Practices: Limited access to a diverse and nutritious diet due to factors such as poverty, food insecurity, and lack of awareness about healthy eating habits.
●Poverty: Economic constraints restrict access to quality food and healthcare services, exacerbating malnutrition.
●Lack of Healthcare: Limited access to healthcare facilities, including maternal and child healthcare services, contributes to malnutrition, especially in rural areas.
●Poor Sanitation: Inadequate sanitation facilities and hygiene practices increase the risk of infections and diseases that impact nutritional status.
|
|
Impact on Health
|
●Child Development: Malnutrition during the critical early years of life can lead to stunted growth, impaired cognitive development, and long-term health issues.
●Increased Vulnerability to Diseases: Malnourished individuals have weakened immune systems, making them more susceptible to infections and diseases.
●Maternal Health Issues: Undernourished mothers face higher risks during pregnancy and childbirth, leading to complications for both the mother and child.
●Rising Non-Communicable Diseases: Overnutrition contributes to the increasing burden of non-communicable diseases such as diabetes, hypertension, and cardiovascular diseases.
|
|
Government Initiatives
|
●Integrated Child Development Services (ICDS): Government program focusing on maternal and child health, providing supplementary nutrition, healthcare, and early childhood education services.
●National Health Mission (NHM): Aims to improve healthcare infrastructure and provide essential healthcare services, including maternal and child healthcare.
●Midday Meal Scheme: Government initiative providing free meals to school children to improve nutritional intake and encourage school attendance.
●Fortification Programs: Efforts to fortify staple foods with essential micronutrients to address deficiencies on a larger scale.
|
|
Challenges
|
●Regional Disparities: Malnutrition rates vary across different states and regions, with some areas facing higher prevalence due to socioeconomic disparities and unequal access to resources.
●Lack of Awareness: Limited understanding of the importance of nutrition and healthcare practices, particularly in rural and marginalized communities.
●Infrastructure Issues: Inadequate healthcare infrastructure, including healthcare facilities and trained healthcare professionals, especially in rural and remote areas, hinders effective intervention and treatment of malnutrition.
●Climate-Related Challenges: Climate variability and environmental factors impact agricultural productivity, affecting food availability and exacerbating food insecurity and malnutrition.
|
|
Future Strategies
|
●Education Programs: Implementing comprehensive nutrition education programs to increase awareness about healthy dietary practices, proper nutrition during different life stages, and the importance of healthcare services.
●Enhanced Healthcare Infrastructure: Investing in improving healthcare infrastructure, including healthcare facilities, equipment, and trained healthcare professionals, particularly in rural and underserved areas.
●Agricultural Reforms: Promoting sustainable agricultural practices, diversification of crops, and improving access to irrigation and agricultural inputs to enhance food production and availability.
●Policy Revisions: Implementing policy reforms addressing socioeconomic factors contributing to malnutrition, such as poverty alleviation measures, social safety nets, and promoting equitable access to resources and opportunities.
|
Conclusion
- The coexistence of undernutrition and obesity in India presents a complex challenge that demands a comprehensive and multifaceted approach. By addressing the root causes of both issues and promoting healthy lifestyles, India can work towards a future where everyone has access to the right kind of food and can lead healthy and productive lives.
Must Read Articles:
CHILD MALNUTRITION: JOINT CHILD MALNUTRITION ESTIMATES: https://www.iasgyan.in/daily-current-affairs/child-malnutrition-joint-child-malnutrition-estimates#:~:text=India%20is%20the%20largest%20country,%25
|
PRACTICE QUESTION
Q. The Indian government provides food subsidies to address food insecurity. However, these programs can sometimes incentivize the consumption of refined carbohydrates over more nutritious options. How to reform subsidy programs to promote both food security and healthy dietary patterns?
|