Description

Disclaimer: Copyright infringement not intended.
Context
- Only 1-2% of the population who need palliative care have access to it in India compared to the global average of 14%- Health Ministry Data.
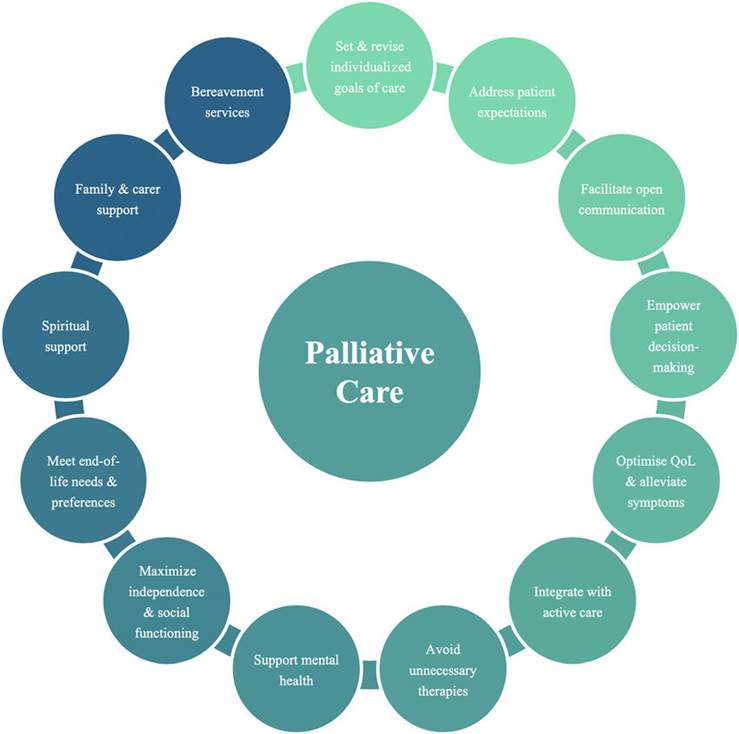
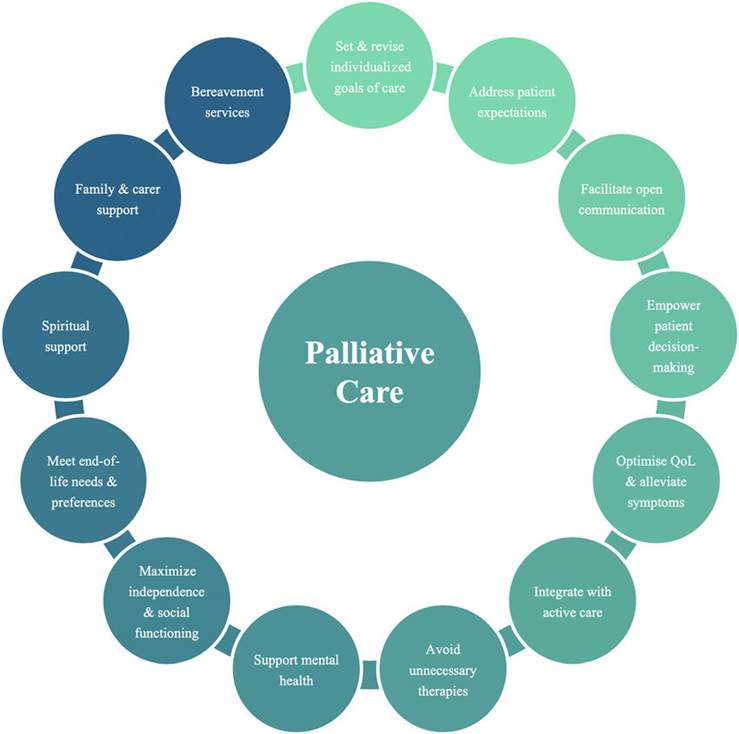
Palliative Care
- Palliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
- Palliative care is required for a wide range of diseases. The majority of adults in need of palliative care have chronic diseases such as cardiovascular diseases, cancer, chronic respiratory diseases, AIDS and diabetes. Many other conditions may require palliative care, including kidney failure, chronic liver disease, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis, neurological disease, dementia, congenital anomalies and drug-resistant tuberculosis.
Insufficient access to palliative care
- Each year an estimated 56.8 million people are in need of palliative care, most of whom live in low- and middle-income countries. For children, 98% of those needing palliative care live in low- and middle-income countries with almost half of them living in Africa.
- Worldwide, a number of significant barriers must be overcome to address the unmet need for palliative care:
- National health policies and systems often do not include palliative care at all;
- Training on palliative care for health professionals is often limited or non-existent; and
- Population access to opioid pain relief is inadequate and fails to meet international conventions on access to essential medicines.
- According to a WHO survey relating to noncommunicable diseases conducted among 194 Member States in 2019: funding for palliative care was available in 68% of countries and only 40% of countries reported that the services reached at least half of patients in need.
Other barriers to palliative care include:
- Lack of awareness among policy-makers, health professionals and the public about what palliative care is, and the benefits it can offer patients and health systems;
- Cultural and social barriers, such as beliefs about death and dying;
- Misconceptions about palliative care, such as that it is only for patients with cancer, or for the last weeks of life; and
- Misconceptions that improving access to opioid analgesia will lead to increased substance abuse.
Situation in India: Health Ministry Data
- India stands at number three in terms of cancer incidence in the world, most States in the country do not even have enabling legislation or policy to integrate palliative care with treatment offered to cancer patients.
- Currently only three States in India (Kerala, Karnataka and Maharashtra) have a palliative care policy. Kerala, Mizoram, Tamil Nadu, Karnataka, Punjab, and Assam report the highest overall crude incidence rates of cancers which is greater than 130 cases per lakh population.
- In a global comparison for organ-wise incidence, the disease burden for head and neck, breast, cervix and ovary cancers in India is higher if not at par with other countries like China, the U.S. and the UK.
- The state of cancer incidence in the country, the financial burden for cancer treatment is highest compared to all diseases, making it unaffordable for over 80% of the population. The cost of single hospitalisation for cancer care is three times that of any other non-communicable disease. Cancer disease burden in India continues to be characterised by poor detection. Late-stage detection coupled with sub-optimal access to quality cancer treatment at affordable prices significantly impacts the outcomes for this disease in the country. As incidence rates continue to rise, deaths due to cancer have remained among the top 5 causes of deaths in India.
- Medical insurance does not play a significant role in hospice and palliative care provision in India.

Way Ahead
- Government needs to undertake efforts to include palliative care packages under reimbursement schemes of government as well as private insurance plans.
- India needs a systematic approach to improving palliative care. These improvements include increasing the workforce, better application of policies, good political support, and educating health care workers and patients requiring palliative treatment.
- Each state needs to develop its own policy that suits its needs and its social and cultural background. Community models for the provision of home-based PC need to be implemented all over the country. Empowerment of family members and volunteers to be effective palliative caregivers might prove to be the most realistic approach for meaningful coverage, especially in rural areas.
- A change in health care to include PC early in the course of cancer care can begin to familiarise the family with PC services, start communication about death earlier in the course of cancer treatment and provide an opportunity for discussion of goals of care among the physician, patient and family.
- Though some major barriers to access to PC in India have been overcome but implementation of created policies and laws still requires massive efforts by both the government system and Non-Government Organisations. Five years after the amendment of NDPS Act in 2014 opioids like oral morphine remain inaccessible for 98% of the population of India.
- There is an acute shortage of trained PC physicians, so clinicians should attend local and national presentations on PC to increase their knowledge base.
- Introduction of palliative medicine into the curriculum of undergraduate education of doctors and nurses is recommended as an efficient way to broaden the base of PC coverage at the national level.
- Research in PC is very much essential to deliver a high-quality palliative care. In fact, many of the developments like megestrol for cancer cachexia, bisphosphonates for pain in bone metastasis, opioids for palliation of breathlessness in terminal illness have come from research in palliative care.
Final Thought
- Future scope for PC in the country lies in the provision of facilities and medicines, sustainability of services, support from the community, government, media and team building for palliative care. Recent declaration by the WHA( World Health Assembly) asking all member states to integrate PC with routine health care comes as a major tool in advocacy and hopefully will boost the current efforts.
https://www.thehindu.com/sci-tech/health/only-1-2-of-population-who-need-palliative-care-have-access-to-it-ficci-report/article66045164.ece