Description
Copyright infringement not intended
Context: According to the data released by the Health Ministry, cancer treatment, emergency care, orthopaedics, and urology (kidney-related diseases) are the top tertiary care specialities treatment received by beneficiaries under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY). The programme has already recorded five crore hospital admissions totalling Rs. 61,501 crore.
Details
- Women account for over 49% of Ayushman card subscribers, and they account for over 48% of total authorised hospital admissions under the AB PM-JAY scheme.
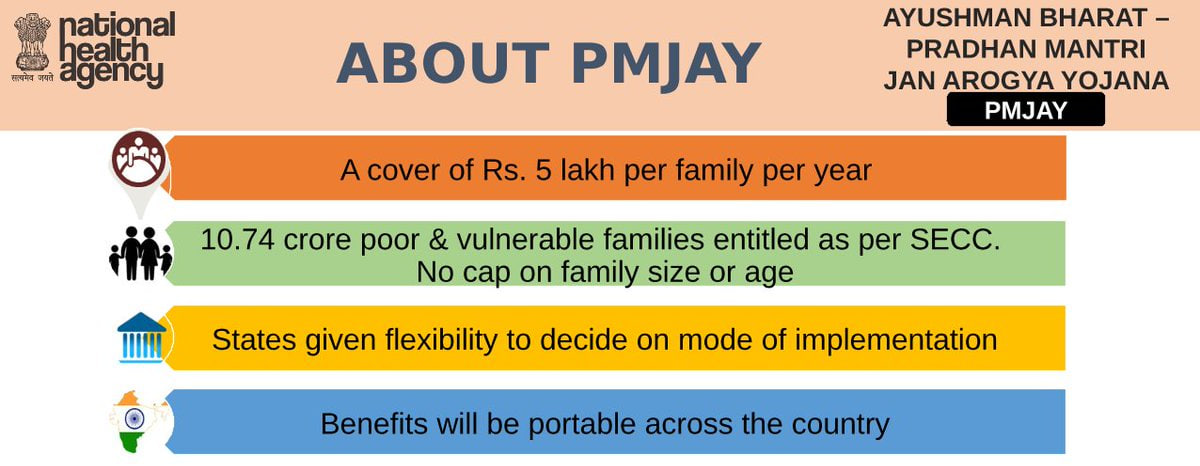
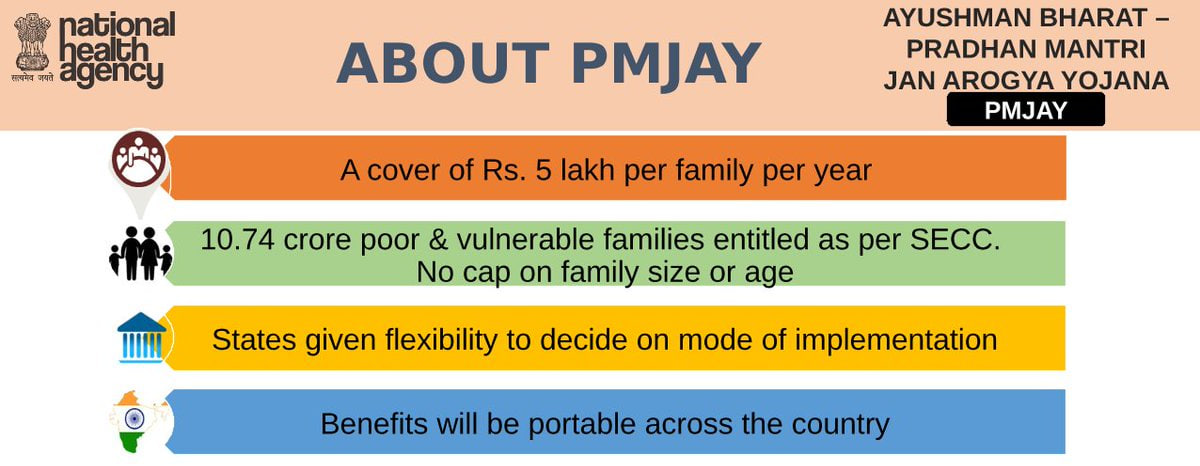
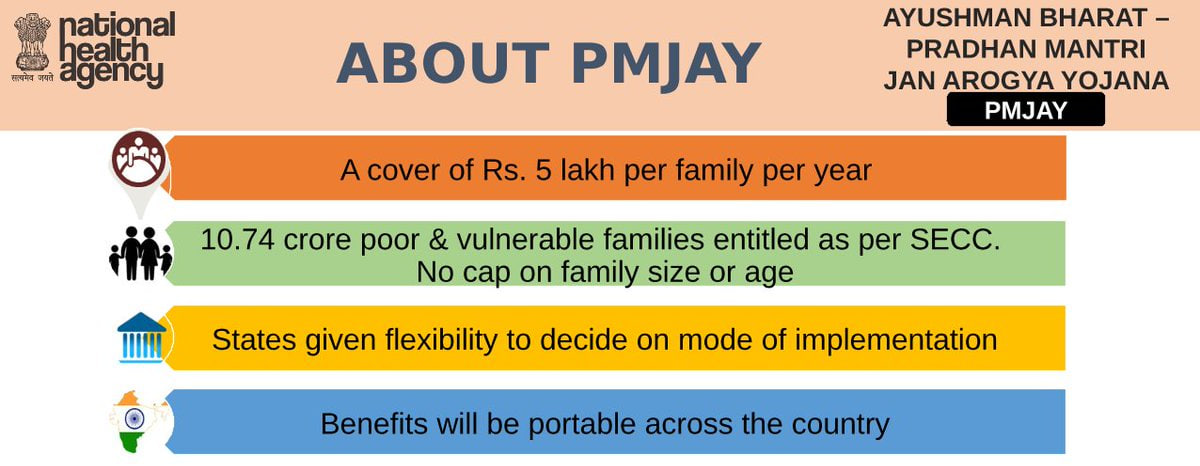
Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY)
About
- AB PM-JAY is the largest health assurance scheme in the world, covering over 10 crore families (approximately 50 crore beneficiaries) that form the bottom 40% of the Indian population.
- The scheme being implemented by the National Health Authority (NHA) provides health cover of ₹5 lahks per family per year for secondary and tertiary care hospitalization.
- The beneficiaries can avail of cashless and paperless treatment at any of the empanelled hospitals across the country.
- The scheme is based on the Socio-Economic Caste Census 2011 (SECC 2011) data, which ensures that no eligible beneficiary is left out.
Health and Wellness Centres
- The other component of Ayushman Bharat is the Health and Wellness Centres (HWCs), which are being established by transforming the existing Sub Centres and Primary Health Centres.
- These centres provide comprehensive primary health care services, including maternal and child health, non-communicable diseases, free essential drugs and diagnostic services, and health promotion and prevention.
Present Status
- Except for Delhi, Odisha, and West Bengal, the AB PM-JAY is being implemented in 33 states and union territories.
- To date, 23.39 crore beneficiaries have been verified and Ayushman cards have been distributed to receive free treatment under the scheme.
- The PM-JAY hospital network spans the country and includes 28,351 institutions, including 12,824 private hospitals.
Significance of AB PM-JAY
- AB PM-JAY is a significant step towards achieving the vision of Universal Health Coverage (UHC), as recommended by the National Health Policy 2017.
- UHC means that all people have access to quality health services that meet their needs without exposing them to financial hardship.
- AB PM-JAY addresses the major barriers to UHC in India, such as high out-of-pocket expenditure, low public spending on health, fragmentation of health services, and lack of health insurance penetration.
- AB PM-JAY is also an important component of Ayushman Bharat, a comprehensive initiative that aims to strengthen the primary, secondary and tertiary levels of health care in India.

Challenges of AB PM-JAY
Identification and verification of beneficiaries
- The SECC 2011 data may not be updated or accurate enough to capture the current socio-economic status of the households. Moreover, there may be issues of duplication, exclusion or inclusion errors in the beneficiary list.
- The scheme relies on Aadhaar-based authentication for verifying the beneficiaries, but not all beneficiaries may have Aadhaar cards or biometric devices at the point of service.
Availability and quality of healthcare providers
- The scheme requires a large network of empanelled hospitals that can provide quality and affordable healthcare services to the beneficiaries. However, there may be a shortage or uneven distribution of such hospitals, especially in rural and remote areas.
- Moreover, there may be variations in the quality and standards of care among different providers, which may affect the outcomes and satisfaction of the beneficiaries.
Fraud and abuse
- The scheme is vulnerable to fraud and abuse by various stakeholders, such as hospitals, intermediaries, beneficiaries or officials.
- Some examples of fraud and abuse are fake enrolment, fake claims, overcharging, unnecessary procedures, denial of service, etc. These practices not only harm the beneficiaries but also drain the financial resources of the scheme.
Monitoring and evaluation
- The scheme requires a robust monitoring and evaluation system that can track the performance and impact of the scheme on various indicators, such as utilization, expenditure, quality, outcomes, etc.
- The system should also be able to detect and prevent any irregularities or anomalies in the data or transactions. However, such a system may be challenging to design and implement given the scale and complexity of the scheme.
Financing and sustainability
- The scheme is funded by both the central and state governments in a 60:40 ratio. However, given the fiscal constraints and competing priorities of both levels of government, there may be issues of adequacy and timeliness of fund allocation and release.
- Moreover, there may be uncertainties about the future demand and cost escalation of healthcare services under the scheme. Therefore, there is a need to ensure adequate and sustainable financing for the scheme in the long run.
To overcome these challenges and ensure the success of AB PM-JAY, some possible ways forward are:
- Strengthening the communication and outreach strategies to increase awareness and information dissemination among the beneficiaries and the general public about the scheme, its features, benefits, entitlements etc.
- Investing in improving the infrastructure and human resources in the public health system, especially at the primary and secondary levels, to enhance the quality and accessibility of health care services for the beneficiaries.
- Building trust and partnership with the private sector by addressing their concerns and grievances, ensuring timely payments, rationalizing package rates, strengthening fraud detection and prevention mechanisms, enhancing quality assurance etc.
- Reducing out-of-pocket expenditure for the beneficiaries by expanding the scope and coverage of the scheme to include more services, drugs and consumables, as well as ensuring no co-payment and balance billing by any hospital.
- Harmonizing and integrating existing health insurance schemes at the central and state levels to create a unified and efficient health care delivery system that avoids confusion and duplication.
- Developing robust monitoring and evaluation systems to measure the impact and outcomes of the scheme on various indicators such as health status, financial protection, equity, quality etc.
Conclusion
- AB PM-JAY is a landmark initiative that has the potential to transform the healthcare scenario in India. However, it requires concerted efforts from all stakeholders - government, private sector, civil society, media etc, to address its challenges and leverage its opportunities. Only then can AB PM-JAY fulfil its promise of providing "Health for All" in India.
Must Read Articles:
Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) Scheme: https://www.iasgyan.in/daily-current-affairs/ayushman-bharat-pradhan-mantri-jan-arogya-yojana-ab-pmjay
|
PRACTICE QUESTION
Q. How can Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) achieve its objectives of providing universal health coverage and improving health outcomes for the poor and vulnerable sections of society? What are the major challenges faced by the scheme and what are the possible solutions to overcome them?
|

https://epaper.thehindu.com/ccidist-ws/th/th_delhi/issues/37961/OPS/GCKBA3SFI.1+G8ABA4QNR.1.html