Description
Copyright infringement not intended
Picture Courtesy: economictimes.indiatimes.com
Context: A study from the University of Manchester has found that people from deprived backgrounds, those with existing health conditions, and those with learning disabilities are at a much higher risk of dying from sepsis.
Details
- The study from the University of Manchester highlights the significant impact of social and health disparities on the risk of sepsis-related mortality.
Key points from the Study
- Socioeconomic Disparities: Individuals from more deprived socioeconomic backgrounds are found to be twice as likely to die from sepsis within 30 days. This emphasizes the importance of addressing social determinants of health in sepsis prevention and treatment.
- Vulnerable Populations: The study identifies specific groups with higher vulnerability to sepsis:
- People with learning disabilities are almost four times more likely to develop sepsis.
- Individuals with liver disease have about three times greater risk.
- Patients with stage 5 chronic kidney disease have more than six times the risk.
- Those with cancer, brain disease, immunosuppressive conditions, and those who have received multiple courses of antibiotics are also at higher risk.
- Awareness and Diagnosis Challenges: The study emphasizes the challenges in diagnosing sepsis, particularly as its symptoms may overlap with other illnesses. This highlights the need for increased awareness among healthcare professionals to ensure early diagnosis and treatment.
- Antibiotic Use: The researchers note a correlation between exposure to multiple courses of antibiotics and an increased risk of sepsis. The reasons for this association are not fully understood, but potential factors include adverse effects on gut bacteria, increased susceptibility to infection, or underlying differences in immune status or comorbidities.
- NHS Challenges: The study comes in the context of challenges within the National Health Service (NHS), including delays in diagnosing and treating sepsis, poor communication, and missed opportunities for follow-up care. The NHS has been urged to improve sepsis awareness and response.
- Call for Action: The study suggests that the findings should guide health professionals worldwide in diagnosing sepsis earlier and initiating treatment sooner. Understanding the social and health factors that contribute to sepsis risk can help address health inequalities.

Sepsis
- Sepsis is a life-threatening condition that occurs when the body's response to an infection injures its tissues and organs. It can lead to shock, multiple organ failure, and death.
- It is a serious medical condition that can be fatal. However, early diagnosis and treatment can improve the chances of survival.
- It can be caused by any type of infection, including bacterial, viral, fungal, or parasitic infections. The most common infections that lead to sepsis are pneumonia, urinary tract infections, and skin infections.
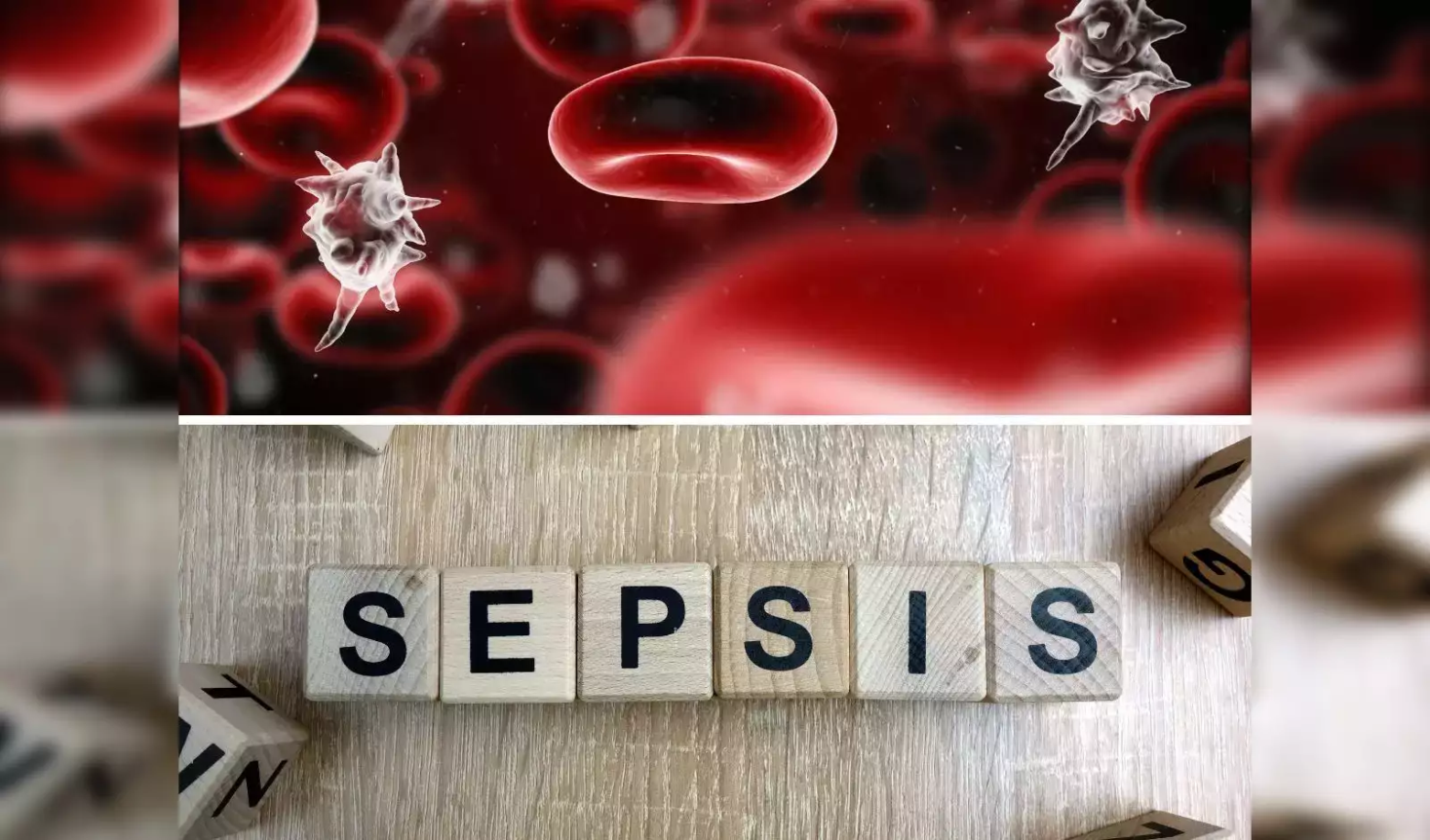
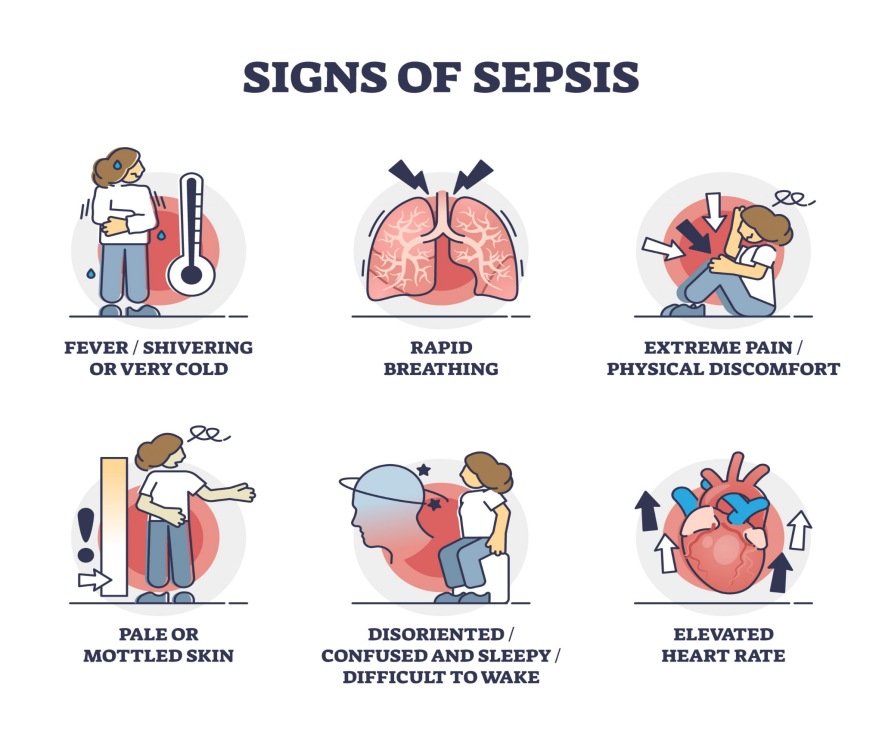
- Symptoms of sepsis can vary depending on the severity of the infection and the individual's overall health. Some common symptoms of sepsis include Fever, Rapid heart rate, Rapid breathing, Confusion, Disorientation, Skin rash, Low blood pressure, and Pain.
Risk factors for Sepsis
- Weakened immune system: People with weakened immune systems, such as those with cancer, HIV/AIDS, or diabetes, are more likely to develop sepsis.
- Young age: Children under the age of 1 year are at higher risk of sepsis.
- Older age: Adults over the age of 65 are also at higher risk of sepsis.
- Chronic illness: People with chronic illnesses, such as chronic obstructive pulmonary disease (COPD), kidney disease, or heart disease, are at higher risk of sepsis.
Diagnosis of sepsis
- Diagnosing sepsis can be difficult because the symptoms can be similar to those of other illnesses.
- Doctors will typically ask about medical history, perform a physical exam, and order laboratory tests.
- Blood tests can measure levels of white blood cells, platelets, and other substances that can help to diagnose sepsis.
Treatment of sepsis
- Treatment for sepsis depends on the severity of the infection and the individual's overall health.
- Antibiotics are used to treat the infection that is causing sepsis.
- Fluids are given to help maintain blood pressure and organ function.
- Vasopressors are medications that help to constrict blood vessels and increase blood pressure.
- Oxygen therapy is given to help improve oxygen levels in the blood.
- Surgery may be needed to remove infected tissue or to drain an abscess.

Conclusion
- The study underscores the importance of a holistic approach to sepsis prevention and treatment, taking into account socioeconomic factors, underlying health conditions, and potential implications of antibiotic use. It also emphasizes the need for improved awareness, diagnosis, and response within healthcare systems.
|
PRACTICE QUESTION
Q. How does the intersection of poverty and disease contribute to a cycle of vulnerability, and what are effective strategies to break this cycle and improve health outcomes in economically disadvantaged communities?
|