Description
Copyright infringement not intended
Picture Courtesy: www.australiawidefirstaid.com.au
Context: The rapid spread of viruses during the COVID-19 pandemic highlights the need for genomic surveillance to track variants. Scientists from the Indian Council of Medical Research-National Institute of Virology have detected the Clade 9 variant of varicella zoster virus (VZV) for the first time in India.
Details
- The Clade 9 variant of the varicella-zoster virus (VZV) has been identified in India for the first time. This virus is responsible for causing chickenpox and herpes zoster (shingles).
- Despite the presence of the Clade 9 variant, there were no significant indications of increased disease severity in the patients. However, in rare cases, VZV infections can lead to severe complications, including central nervous system involvement.
Shingles
- Shingles, also known as herpes zoster, is a viral infection caused by the varicella-zoster virus (VZV). This is the same virus responsible for chickenpox.
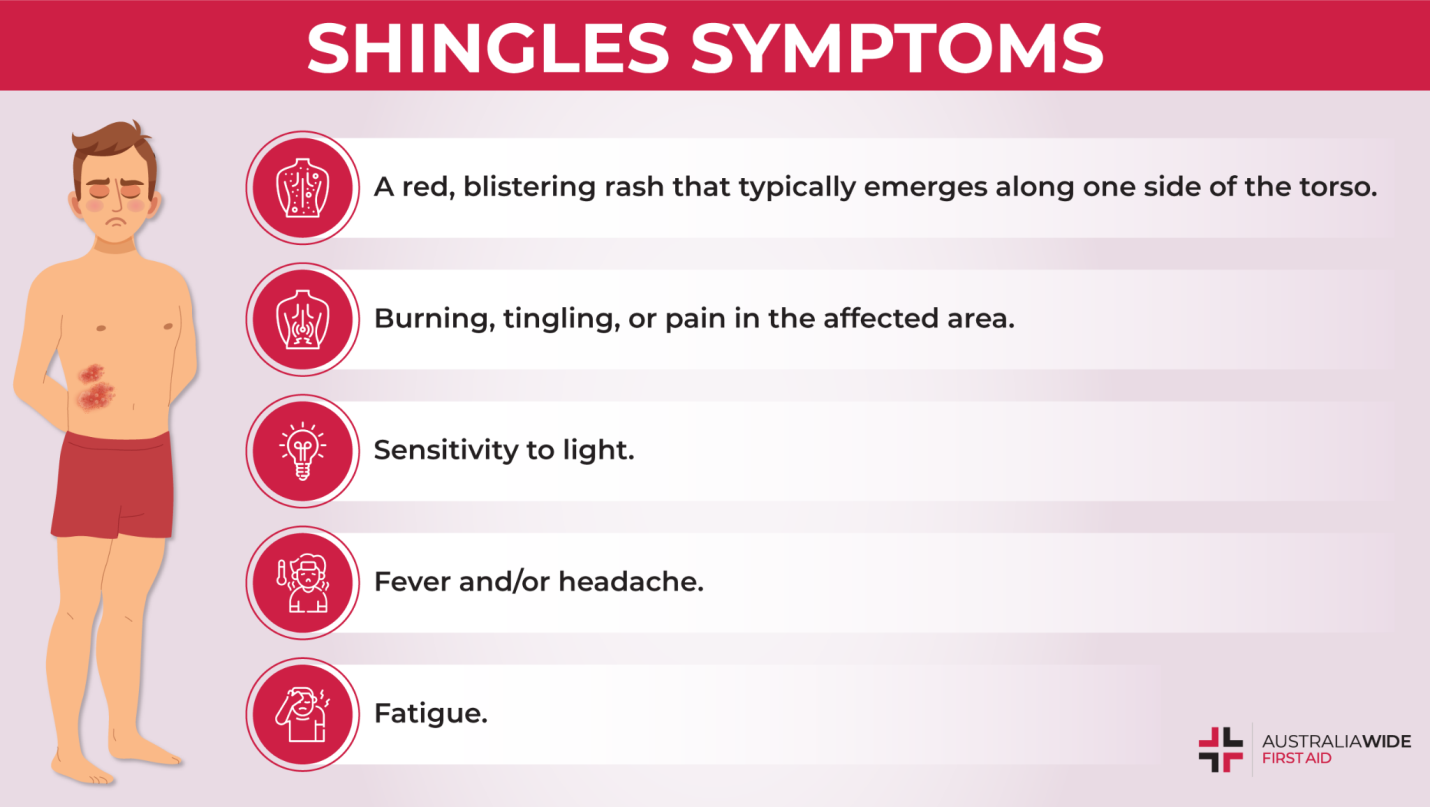
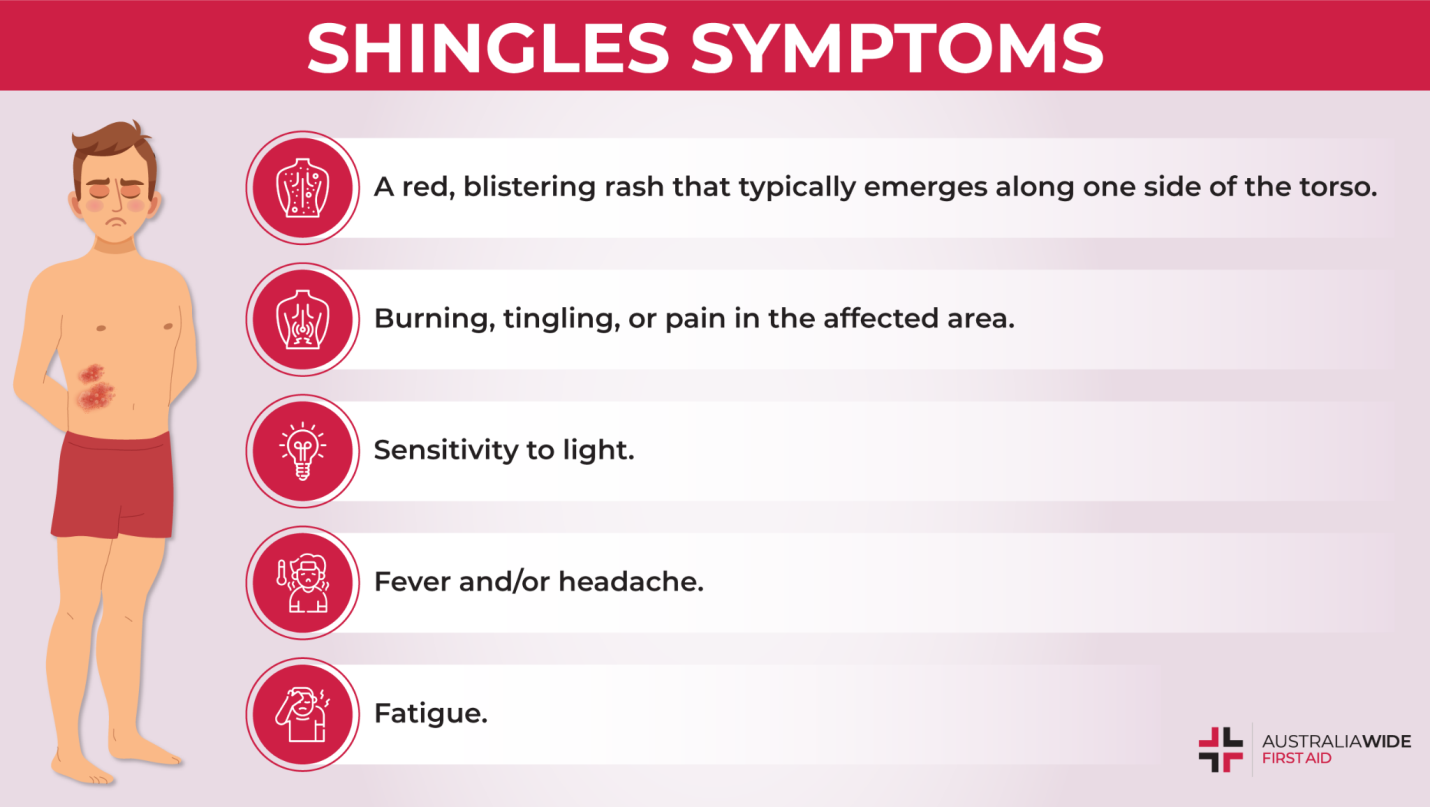
Symptoms (Signs of Shingles)
- Painful Rash: The hallmark symptom of shingles is a painful rash. This rash is characterized by red patches that evolve into fluid-filled blisters. It typically appears on one side of the body or face and follows the path of a nerve. The pain can range from mild to severe and is often described as burning, stabbing, or shooting.
- Itching and Tingling: Before the rash becomes visible, many individuals experience itching, burning, or tingling sensations in the area where the rash will eventually appear. These sensations can be uncomfortable and are often an early warning sign of shingles.
- Flu-Like Symptoms: In addition to the rash and localized pain, some people with shingles may experience flu-like symptoms. These can include fever, headache, and fatigue. These symptoms are not as prominent as the rash and pain but can contribute to overall discomfort.
- Blisters: The rash progresses from red patches to small, fluid-filled blisters. These blisters are fragile and can break open, oozing fluid. Over time, the blisters crust over and begin to heal. The entire process can take several weeks.
- Postherpetic Neuralgia (PHN): PHN is a potentially debilitating complication of shingles. It occurs when the pain associated with shingles persists long after the rash has healed. This chronic nerve pain can last for months or even years and can significantly impact an individual's quality of life.
Impact (Consequences of Shingles)
- Pain: The pain associated with shingles can be one of the most significant and distressing consequences. This pain is often severe and can range from burning and stabbing sensations to a constant ache. It can affect daily activities such as walking, dressing, and sleeping. The pain can persist throughout the active phase of the rash and, in some cases, continue even after the rash has healed. This long-lasting pain is referred to as postherpetic neuralgia (PHN).
- Scarring: Shingles blisters can leave scars, especially if they become infected or are scratched excessively. These scars can be a reminder of the shingles episode and may take time to fade or may be permanent.
- Postherpetic Neuralgia (PHN): PHN is a common and often long-lasting complication of shingles. It occurs when the nerves in the affected area continue to send pain signals to the brain long after the rash has healed. PHN can be extremely debilitating and may last for months or even years. It can greatly impact an individual's quality of life, leading to chronic pain and discomfort.
- Eye Complications: Shingles can be particularly concerning when it occurs near the eyes, a condition known as herpes zoster ophthalmicus. This can lead to a range of eye-related complications, including:
- Corneal Damage: Shingles near the eye can cause corneal ulcers or scarring, potentially leading to vision problems or even blindness.
- Iris Inflammation: Inflammation of the iris (iritis) can occur, causing eye pain and light sensitivity.
- Glaucoma: Shingles can increase the risk of developing glaucoma, a condition characterized by increased pressure within the eye.
- Retinal Damage: In severe cases, shingles can damage the retina, affecting vision.
Challenges associated with shingles
- Misdiagnosis: Misdiagnosis of shingles can be a significant challenge. The symptoms of shingles, especially in the early stages, can resemble those of other skin conditions or ailments. Common misdiagnoses include mistaking shingles for contact dermatitis, insect bites, or fungal infections. This misdiagnosis can lead to delayed treatment, potentially allowing the virus to progress, resulting in more severe symptoms and complications.
- Complications: Shingles can lead to various complications, and these can significantly impact an individual's quality of life. Two notable complications have been previously mentioned:
- Postherpetic Neuralgia (PHN): PHN is one of the most common and challenging complications of shingles. It causes long-lasting, chronic nerve pain in the area previously affected by the rash. Managing this pain can be difficult and may require ongoing medical treatment.
- Bacterial Skin Infections: Scratching the shingles rash can introduce bacteria into the blisters, leading to bacterial skin infections. These infections can further exacerbate discomfort and require additional medical attention.
- Vaccination Coverage: Ensuring that at-risk populations receive the shingles vaccine can be a challenge. There are several factors contributing to this challenge:
- Vaccine Availability: The shingles vaccine may not always be readily available in all healthcare settings or regions, leading to disparities in access.
- Awareness: Some individuals may not be aware of the importance of shingles vaccination or may not realize they are at risk.
- Healthcare Providers: Some healthcare providers may not consistently offer or recommend the vaccine to eligible patients.
Addressing these challenges requires a multifaceted approach, including raising awareness about shingles and its complications, improving access to vaccination, educating healthcare providers about the importance of vaccination, and ensuring that vaccines are readily available in healthcare settings.
Cure and Treatment
Antiviral Medications
- Early treatment with antiviral medications is a key strategy in managing shingles. These medications include acyclovir, valacyclovir, and famciclovir.
- Antiviral drugs can help:
- Reduce the severity and duration of the shingles rash.
- Alleviate pain and discomfort.
- Lower the risk of complications, including postherpetic neuralgia (PHN).
- To be most effective, antiviral medications should ideally be started within 72 hours of the rash's onset, but they may still provide some benefit if initiated later.
Pain Management
- Pain management is an integral part of shingles treatment, as the pain can be severe and persistent.
- Over-the-Counter (OTC) Pain Medications: Non-prescription pain relievers like acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil) can help alleviate pain.
- Prescription Pain Medications: In some cases, stronger prescription pain medications may be necessary, especially if the pain is severe.
Topical Creams
- Topical creams or ointments containing ingredients like capsaicin or lidocaine can be applied directly to the affected area to provide localized pain relief.
- These topical treatments can help numb the skin and reduce discomfort, particularly for those with milder cases of shingles.
Postherpetic Neuralgia (PHN) Management
- Managing postherpetic neuralgia (PHN), which is persistent nerve pain after the shingles rash has healed, may require specialized treatment. Options include:
- Nerve Blocks: Injection of medication near the affected nerves can provide temporary relief from PHN.
- Antidepressants: Certain antidepressant medications, such as tricyclic antidepressants or selective serotonin and norepinephrine reuptake inhibitors (SNRIs), can help manage nerve pain.
- Antiseizure Medications: Drugs like gabapentin or pregabalin are sometimes used to reduce nerve-related pain.
Vaccination
- The shingles vaccine, also known as the herpes zoster vaccine, is a preventive measure that can significantly reduce the risk of developing shingles or lower the severity of symptoms.
- The vaccine is recommended for individuals aged 50 and older. There are two shingles vaccines available: Shingrix and Zostavax. Shingrix is generally preferred because it is more effective.
- Vaccination is especially important for those at higher risk of shingles, such as older adults or individuals with weakened immune systems.
Summary
- Shingles is a painful viral infection caused by VZV, and its impact can be significant, including chronic pain and complications like PHN. Early diagnosis and treatment with antiviral medications are essential, and vaccination is a key preventive measure. Public education, research, and efforts to control the virus's spread are vital components of the way forward in managing shingles.
|
PRACTICE QUESTION
Q. The term “Shingles” is frequently seen in the news, it is related with:
1.Malware
2.Web Browser
3.Viral infection
4.New Variant of Covid-19
Answer: C
Explanation:
Shingles, also known as herpes zoster, is a viral infection caused by the varicella-zoster virus (VZV). This virus is the same one responsible for causing chickenpox. After a person has had chickenpox, the virus remains dormant in the nerve cells of the body. Later in life, the virus can reactivate, leading to the development of shingles.
Shingles is characterized by a painful and often blistering rash that typically appears on one side of the body or face. This rash follows the path of a nerve and can be associated with itching, burning, or tingling sensations. Additional symptoms may include fever, headache, and fatigue.
|
https://indianexpress.com/article/cities/pune/in-a-first-scientists-identify-variant-of-chickenpox-causing-virus-icmr-niv-study-8929749/