Description
Disclaimer: Copyright infringement not intended.
Context
- An estimated 10.6 million people fell ill with tuberculosis (TB) in 2021, an increase of 4.5% from 2020, and 1.6 million people died from TB - World Health Organization’s 2022 Global TB report.

Report
- This is the first time in many years an increase has been reported in the number of people falling ill with TB and drug resistant TB.
- TB services are among many others disrupted by the COVID-19 pandemic in 2021, but its impact on the TB response has been particularly severe. Ongoing conflicts across Eastern Europe, Africa and the Middle East have further exacerbated the situation for vulnerable populations.
- Many people with TB were not diagnosed and treated. The reported number of people newly diagnosed with TB fell from 7.1 million in 2019 to 5.8 million in 2020. There was a partial recovery to 6.4 million in 2021, but this was still well below pre-pandemic levels.
- Reductions in the reported number of people diagnosed with TB suggest that the number of people with undiagnosed and untreated TB has grown, resulting first in an increased number of TB deaths and more community transmission of infection and then, with some lag-time, increased numbers of people developing TB.
- The number of people provided with treatment for RR-TB and multidrug-resistant TB (MDR-TB) has also declined between 2019 and 2020.
- The report notes a decline in global spending on essential TB services from US$6 billion in 2019 to US$5.4 billion in 2021, which is less than half of the global target of US$13 billion annually by 2022.
About Tuberculosis (TB)
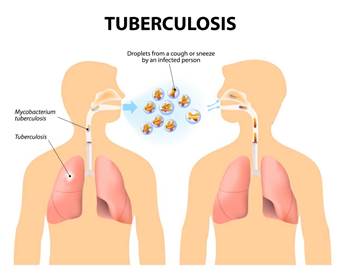
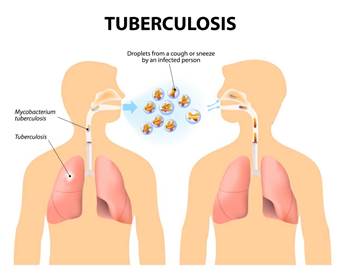
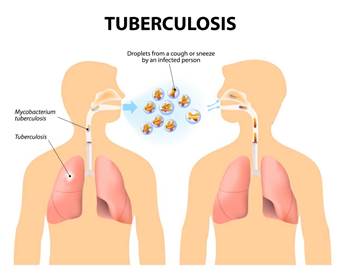
- Tuberculosis (TB) is a potentially serious infectious disease that mainly affects the lungs.
- The ‘Mycobacterium tuberculosis’bacteria that cause TB are spread when an infected person coughs or sneezes.
- Most people infected with the bacteria that cause tuberculosis don't have symptoms. When symptoms do occur, they usually include a cough (sometimes blood-tinged), weight loss, night sweats and fever.
- Treatment isn't always required for those without symptoms. Patients with active symptoms will require a long course of treatment involving multiple antibiotics.
- As in the previous 10 years, most of the funding used in 2021 (79%) was from domestic sources. In other low- and middle-income countries, international donor funding remains crucial. The main source is the Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund). The United States Government is the largest contributor of funding to the Global Fund and is also the largest bilateral donor; overall, it contributes close to 50% of international donor funding for TB.
Present Status of TB in India
- Tuberculosis is one of India's major public health problems. According to World Health Organisation (WHO) estimates, India has the world's largest tuberculosis epidemic.
- In 2020, India accounted for 26% of the incident TB cases across the globe.
- India has an incidence rate of 192 cases per 100,000 of population.
- India accounted for 38% of global TB deaths among HIV-negative people and for 34% of the combined total number of TB deaths in HIV-negative and HIV-positive people.
- Further in 2020, India accounted for 24% of the global gap between estimated TB incidence and the number of people newly diagnosed with TB and reported.
Global TB targets
- In 2014 and 2015, all Member States of WHO and the UN adopted the UN Sustainable Development Goals (SDGs) and WHO’s End TB Strategy. The SDGs and End TB Strategy both include targets and milestones for large reductions in TB incidence, TB deaths and costs faced by TB patients and their households.
- In 2018, countries convened at the United Nations (UN) high-level meeting on TB committed to speed up work towards ambitious targets to treat an additional 40 million people with TB and provide preventive treatment to at least 30 million people at risk of developing the disease by 2022.
Steps taken by the Government
- In 2020, the Indian government made statements to eliminate tuberculosisfrom the country by 2025 through its National TB Elimination Program.
- Interventions in this program include major investment in health care.
- Providing supplemental nutrition credit through the Nikshay Poshan Yojana.
- Organizing a national epidemiological survey for tuberculosis.
- Organizing a national campaign to tie together the Indian government and private health infrastructure for the goal of eliminating the disease.
- The ministry's commitment to eliminating tuberculosis in the country by 2025.
- As part of its efforts to eliminate tuberculosis, the Union Government changed the name of Revised National Tuberculosis Control Program (RNTCP) to National Tuberculosis Elimination Program (NTEP) in December 2019.
Details of Nikshay Poshan Yojana
- The Nikshay Poshan Yojana entitles every tuberculosis (TB) patient, seeking treatment in either the public or private sector, to a direct benefit transfer (DBT) of Rs 500 per month for nutritional needs. It was launched in April 2018 and until February 2022, around Rs 1,488 crore has been paid to 5.73 million notified beneficiaries.
- However, data from the latest India TB Report 2022, released by the Union Ministry of Health and Family Welfare in March 2022, shows that only 62.1 per cent of 2.1 million notified cases across the country received at least one payment in 2021.
- In Delhi, which has the highest burden of all forms of TB at 747 cases per 100,000 people, only 30.2 per cent of patients have got at least one DBT.
- Other poor performers are Punjab (31.8 per cent), Jharkhand (40.1 per cent), Maharashtra (46.6 per cent), Bihar (45.8 per cent), Rajasthan (55.9 per cent) and Uttar Pradesh (58.7 per cent). In the North East, Manipur (4.2 per cent) and Meghalaya (23.7 per cent) fared the worst.
Challenges in implementing the Scheme
- Studies on the scheme since its inception highlight several hurdles in the DBT process. One 2018 paper in the Indian Journal of Tuberculosis, found that “non-availability of bank accounts and unlinked bank accounts were some challenges faced by both health providers and patients.”
- Another 2020 study published in the Journal of Family Medicine and Primary Care underlines lack of communication, stigma, illiteracy and the multi-step approval process as key hurdles.
- States have their own nutritional support schemes, but caveats remain here too; for instance, some schemes are only for patients showing resistance to TB drugs.
Concern
- India has set a target to eliminate TB by 2025.Experts believe that to reach this goal, the country must go beyond the medical aspects.
- Undernutrition is a major risk factor that drives TB, acknowledges the World Health Organization. The condition accounts for nearly 34 per cent of all cases.
Final thoughts
- The government needs to take stock of where the bottlenecks are. There is no point in pouring more money into a failing system.
- Any investment in diagnostic treatments is irrelevant if people fighting TB are living on an empty stomach. It affects the poorest populations and almost every family is in financial distress due to medical costs and lost wages.
- This distress can worsen food insecurity. A broader approach is needed to prevent TB, and it should include food support for those in close contact with the patientas they are also at high risk of contracting the disease.
- Drug-resistant tuberculosis remains a public health crisis, and ongoing surveillance of the burden is essential to mounting an effective response. Accurate diagnosis and treatment of tuberculosis, including drug-resistant forms, should be available and accessible to all who need it.
- Closing gaps in the detection of drug-resistant tuberculosis requires investment in laboratory capacity, sample transport systems, and data connectivity solutions. To improve detection requires a multistep process, first requiring improved bacteriological confirmation among presumptive cases of pulmonary tuberculosis.
- Efforts are needed to minimise the emergence of resistance to the first new drugs to be made available for the treatment of tuberculosis. Early detection of resistance relies on investment in research and development of new molecular tools.
Final Thoughts
- The Global Project on Anti-Tuberculosis Drug Resistance Surveillance serves to guide the development and expansion of the surveillance of antimicrobial resistance among other pathogens.
- Nonetheless, the global epidemic of drug-resistant tuberculosis remains a public health threat, with the COVID-19 pandemic reversing years of progress.
- Urgent investment is needed from governments, donors, the commercial sector, academic institutions, non-governmental organisations, and other stakeholders.
https://www.who.int/news/item/27-10-2022-tuberculosis-deaths-and-disease-increase-during-the-covid-19-pandemic#:~:text=An%20estimated%2010.6%20million%20people,Organization's%202022%20Global%20TB%20report.
https://indianexpress.com/article/explained/explained-politics/aap-wants-lakshmi-ganesh-on-currency-who-designs-rupee-notes-and-how-8231728/