Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now


Different methods of testing are being experimented in the country to trace COVID-19 infection.
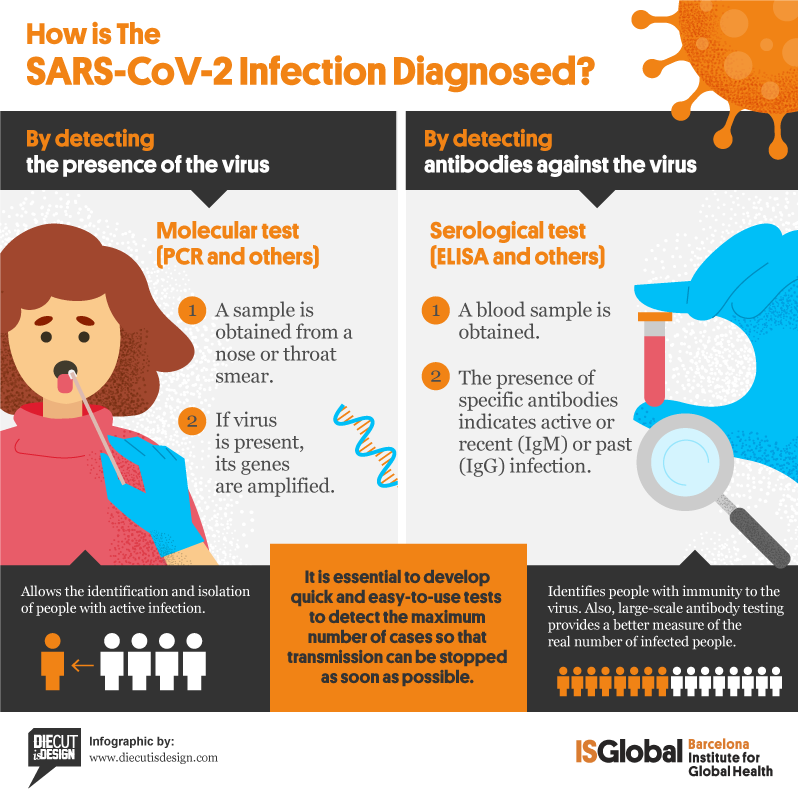
There are mainly three kinds of tests available for COVID-19: Molecular Tests, antigen tests and antibody tests.
About the test
The Molecular test, commonly known as the RT-PCR test, is a method of testing that is used to directly detect the presence of the virus in the sample. The test detects the virus’s RNA, which is the genetic material of the virus. The first step in this test is to convert this RNA to DNA using an enzyme known as the reverse transcriptase. The PCR testing then detects this DNA. Hence, the name RT-PCR. These are also known as the diagnostic test and nucleic acid amplification test (NAAT).
How the sample is taken?
A nasal or throat swab sample is taken.
Time taken to get results
Results are given the same day or within 2-3 days.
Are they accurate?
These tests are the most accurate. They have a high sensitivity and specificity.
What it shows?
These tests help diagnose the active coronavirus infection. If the virus is present in the sample, the test is positive but a negative test doesn’t necessarily mean that you cannot be infected, you might have taken the test in the early days.
What it cannot show?
It fails to show if you ever had COVID-19 in the past.
Cost of RT-PCR test
Cost of the antibody test kit is somewhere between Rs 2000- Rs 3000.
Not every laboratory in the country can conduct a COVID-19 test as the virus is highly contagious. Only NABL (National Accreditation Board for Testing and Calibration Laboratories) accredited laboratories approved by ICMR are equipped to handle the COVID-19 samples.
About the test
A COVID-19 antigen refers to any foreign matter or viral proteins in the body that triggers an immune response. This test helps identify the antigens related to the COVID-19 virus. Antigen test, also known as rapid antigen test, is a rapid diagnostic test that gives results faster than molecular tests. But there is a drawback, antigen tests have a higher chance of missing an active infection.
How the sample is taken?
Usually,anasal or throat swab sample is taken.
Time taken to get results
Since it is a rapid test, results are delivered in 1 hour or less.
What it shows?
These tests help diagnose active coronavirus in the sample.
What it cannot show?
The Antigen test might miss an active coronavirus infection in comparison to RT-PCR tests.
Cost of COVID-19
Antigen test- Cost of the COVID-19 antigen test kit is somewhere between Rs 400- Rs 500
.jpg)
About the test
COVID-19 Antibody tests, also known as, Serology test, serological test, or Serology blood test, are screening tests for COVID-19 antibodies in the blood. It tells if a patient is previously infected with the virus that causes COVID-19. The antibody test does not look for the active virus but checks whether one’s immune system has responded to the infection.
How the sample is taken?
It is tested by drawing the blood sample.
Time taken to get results
Results are delivered either the same day or in 1-3 days.
What it shows
This test helps to find out if you were infected with the virus causing COVID-19 in the past and now have antibodies against it.
What it cannot show
A COVID-19 antibody test may not show if you have an active virus in your body causing COVID-19 infection.
Cost of Antibody test
The cost of COVID-19 antibody test kit is somewhere between Rs 500-Rs 600.
Coronaviruses constitute the subfamily Orthocoronavirinae, in the family Coronaviridae, order Nidovirales, and realm Riboviria.
They are enveloped viruses with a positive-sense single-stranded RNA genome and a nucleocapsid of helical symmetry. The genome size of coronaviruses ranges from approximately 26 to 32 kilobases, one of the largest among RNA viruses.
Coronaviruses are named for the crown-like spikes on their surface. There are four main sub-groupings of coronaviruses, known as alpha, beta, gamma, and delta.
Human coronaviruses were first identified in the mid-1960s. The seven coronaviruses that can infect people are:
Common Human Coronaviruses
229E (alpha coronavirus)
NL63 (alpha coronavirus)
OC43 (beta coronavirus)
HKU1 (beta coronavirus)
Other human coronaviruses
MERS-CoV (the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS)
SARS-CoV (the beta coronavirus that causes severe acute respiratory syndrome, or SARS)
SARS-CoV-2 (the novel coronavirus that causes coronavirus disease 2019, or COVID-19)
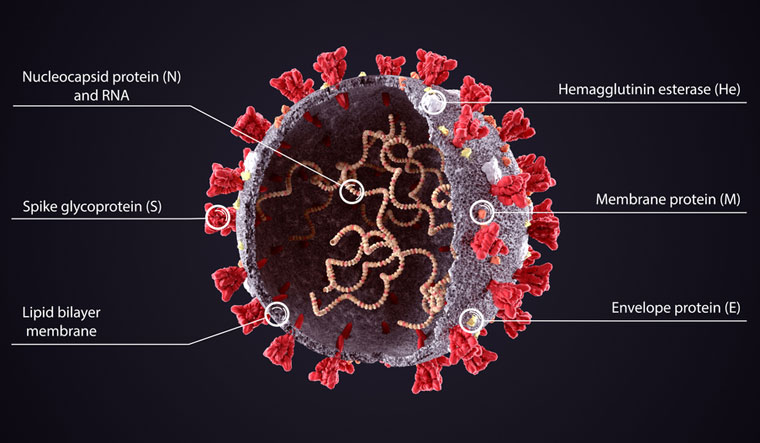
At their core, coronaviruses contain a genetic blueprint called RNA (beige), similar to DNA. The single-stranded RNA acts as a molecular message that enables production of proteins needed for other elements of the virus.
Bound to this string of RNA are nucleoproteins— (dark blue discs)—proteins that help give the virus its structure and enable it to replicate.

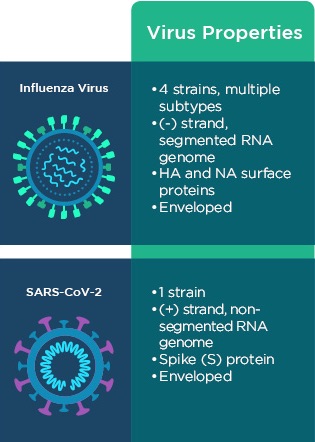
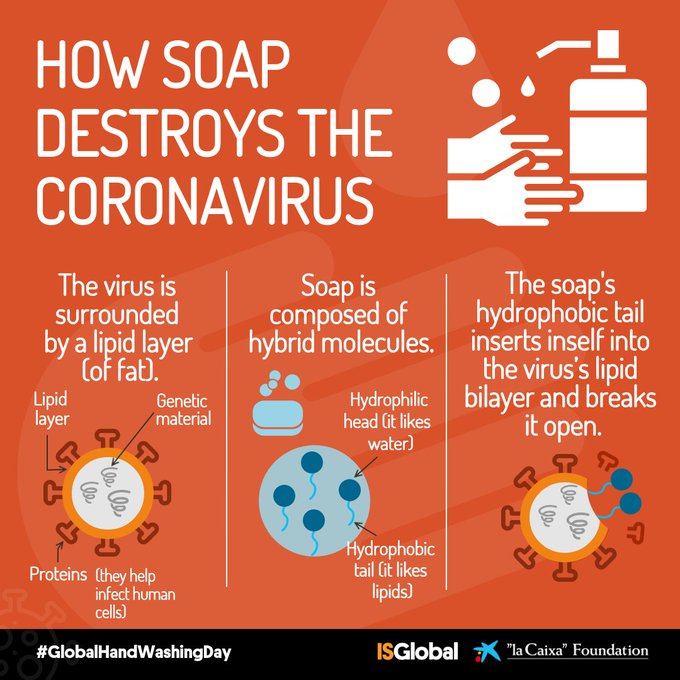
Encapsulating the RNA genome is the viral envelope (teal), which protects the virus when it is outside of a host cell. This outer envelope is made from a layer of lipids, a waxy barrier containing fat molecules. As well as protecting the precious genetic cargo, this layer anchors the different structural proteins needed by the virus to infect cells. Envelope proteins (dark blue dots) embedded in this layer aid the assembly of new virus particles once it has infected a cell.
The bulbous projections seen on the outside of the coronavirus are spike proteins (red-orange). This fringe of proteins gives the virus its crown-like appearance under the microscope, from which the Latin name corona is derived. The spike proteins act as grappling hooks that allow the virus to latch onto host cells and crack them open for infection. Like all viruses, coronaviruses are unable to thrive and reproduce outside of a living host.
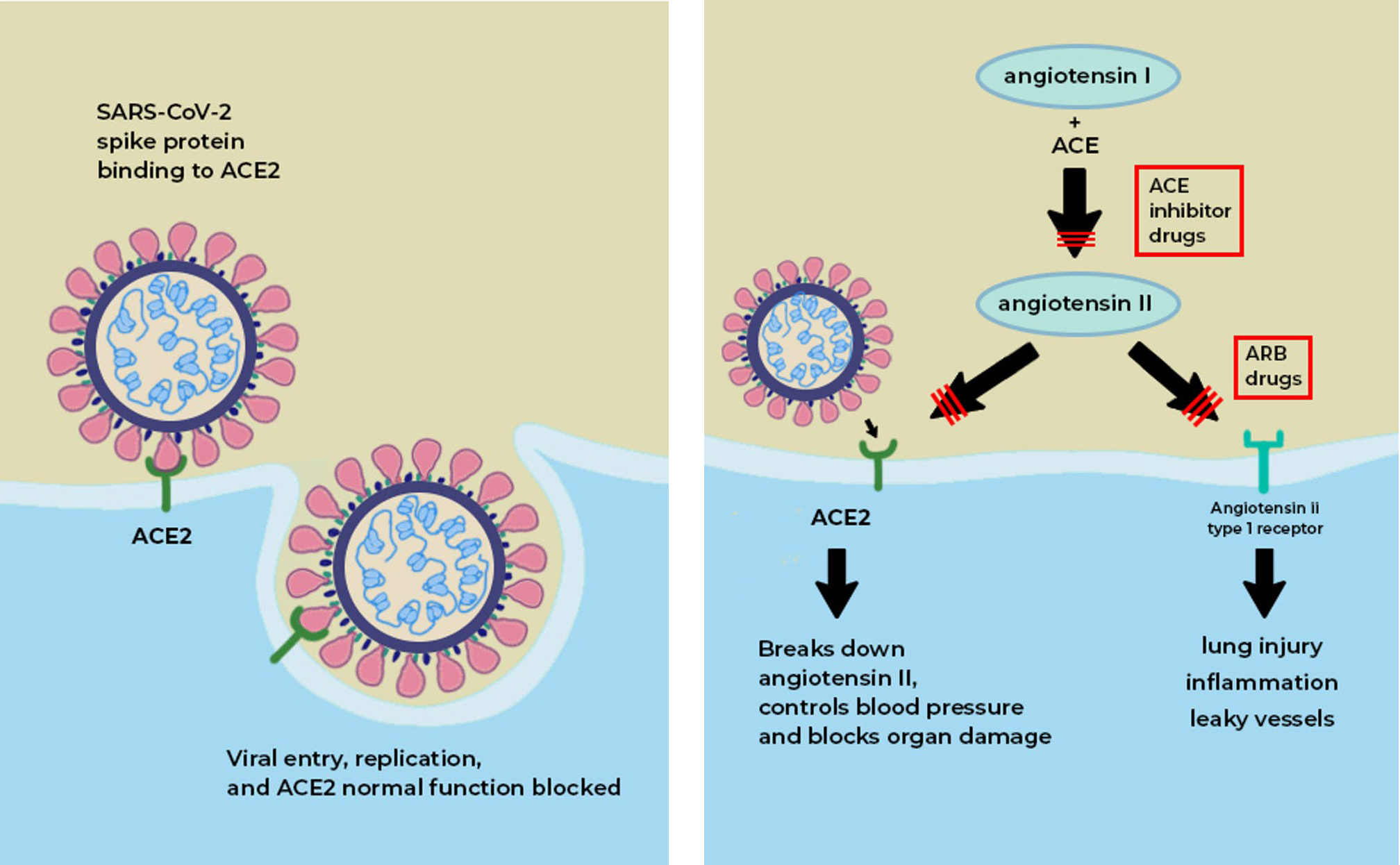
What is the ACE2 receptor?
ACE2 acts as the receptor for the SARS-CoV-2 virus and allows it to infect the cell.
ACE2 is a protein on the surface of many cell types. It is an enzyme that generates small proteins – by cutting up the larger protein angiotensinogen – that then go on to regulate functions in the cell.
Using the spike-like protein on its surface, the SARS-CoV-2 virus binds to ACE2 – like a key being inserted into a lock – prior to entry and infection of cells. Hence, ACE2 acts as a cellular doorway – a receptor – for the virus that causes COVID-19.
Where in the body is it found?
ACE2 is present in many cell types and tissues including the lungs, heart, blood vessels, kidneys, liver and gastrointestinal tract. It is present in epithelial cells, which line certain tissues and create protective barriers.
The exchange of oxygen and carbon dioxide between the lungs and blood vessels occurs across this epithelial lining in the lung. ACE2 is present in epithelium in the nose, mouth and lungs. In the lungs, ACE2 is highly abundant on type 2 pneumocytes, an important cell type present in chambers within the lung called alveoli, where oxygen is absorbed and waste carbon dioxide is released.
What is the normal role ACE2 plays in the body?
The ACE enzyme converts angiotensin I into angiotensin II. The main role of ACE2 is to break down angiotensin II into molecules that counteract angiotensin II’s harmful effects; but if the virus occupies the ACE2 ‘receptor’ on the surface of cells, then its role is blunted. Drugs called ACE inhibitors inhibit the formation of angiotensin II, which would otherwise interact with the angiotensin type 1 receptor to produce tissue damage and inflammation.
ACE2 is a vital element in a biochemical pathway that is critical to regulating processes such as blood pressure, wound healing and inflammation, called the renin-angiotensin-aldosterone system (RAAS) pathway.
ACE2 helps modulate the many activities of a protein called angiotensin II (ANG II) that increases blood pressure and inflammation, increasing damage to blood vessel linings and various types of tissue injury. ACE2 converts ANG II to other molecules that counteract the effects of ANG II.
Of greatest relevance to COVID-19, ANG II can increase inflammation and the death of cells in the alveoli which are critical for bringing oxygen into the body; these harmful effects of ANG II are reduced by ACE2.
When the SARS-CoV-2 virus binds to ACE2, it prevents ACE2 from performing its normal function to regulate ANG II signaling. Thus, ACE2 action is “inhibited,” removing the brakes from ANG II signaling and making more ANG II available to injure tissues. This “decreased braking” likely contributes to injury, especially to the lungs and heart, in COVID-19 patients.
Does everyone have the same number of ACE2 on their cells?
No. ACE2 is present in all people but the quantity can vary among individuals. Evidence suggests that ACE2 may be higher in patients with hypertension, diabetes and coronary heart disease. Studies have found that a lack of ACE2 (in mice) is associated with severe tissue injury in the heart, lungs and other tissue types. Also, t men have higher concentrations of angiotensin-converting enzyme 2 (ACE2) than women.
Does the quantity of receptors determine whether someone gets more or less sick?
This is unclear. The SARS-CoV-2 virus requires ACE2 to infect cells but the precise relationship between ACE2 levels, viral infectivity and severity of infection are not well understood.
Even so, aside from its ability to bind the SARS-CoV-2 virus, ACE2 has protective effects against tissue injury, by mitigating the pathological effects of ANG II.
When the amount of ACE2 is reduced because the virus is occupying the receptor, individuals may be more susceptible to severe illness from COVID-19. That is because enough ACE2 is available to facilitate viral entry but the decrease in available ACE2 contributes to more ANG II-mediated injury. In particular, reducing ACE2 will increase susceptibility to inflammation, cell death and organ failure, especially in the heart and the lung.

Which organs are most severely damaged by SARS-CoV-2?
The lungs are the primary site of injury by SARS-CoV-2 infection, which causes COVID-19. The virus reaches the lungs after entry in the nose or mouth.
ANG II drives lung injury. If there is a decrease in ACE2 activity (because the virus is binding to it), then ACE2 can’t break down the ANG II protein, which means there is more of it to cause inflammation and damage in the body.
The virus also impacts other tissues that express ACE2, including the heart, where damage and inflammation (myocarditis) can occur. The kidneys, liver and digestive tract can also be injured. Blood vessels may also be a site for damage.
In a recent research paper, it has been found that the key factor that determines severity of damage in patients with COVID-19 is abnormally high ANG II activity.
What are ACE inhibitors? Are they a possible treatment or prophylactic for SARS-CoV-2?
Angiotensin converting enzyme (ACE, aka ACE1) is another protein, also found in tissues such as the lung and heart, where ACE2 is present. Drugs that inhibit the actions of ACE1 are called ACE inhibitors. Examples of these drugs are ramipril, lisinopril, and enalapril. These drugs block the actions of ACE1 but not ACE2.
By inhibiting ACE1, ACE inhibitors reduce the levels of ANG II and its ability to increase blood pressure and tissue injury. ACE inhibitors are commonly prescribed for patients with hypertension, heart failure and kidney disease.
Another commonly prescribed class of drugs, angiotensin receptor blockers (ARBs, e.g., losartan, valsartan, etc.) have similar effects to ACE inhibitors and may also be useful in treating COVID-19.
The WHO has estimated an incubation period (between infection and symptom onset) of 2 to 14 days, although most people develop symptoms between 5 and 7 days.
© 2024 iasgyan. All right reserved